A Computerized Clinical Decision Support System as a Means of Implementing Depression Guidelines
Abstract
The authors describe the history and current use of computerized systems for implementing treatment guidelines in general medicine as well as the development, testing, and early use of a computerized decision support system for depression treatment among "real-world" clinical settings in Texas. In 1999 health care experts from Europe and the United States met to confront the well-documented challenges of implementing treatment guidelines and to identify strategies for improvement. They suggested the integration of guidelines into computer systems that is incorporated into clinical workflow. Several studies have demonstrated improvements in physicians' adherence to guidelines when such guidelines are provided in a computerized format. Although computerized decision support systems are being used in many areas of medicine and have demonstrated improved patient outcomes, their use in psychiatric illness is limited. The authors designed and developed a computerized decision support system for the treatment of major depressive disorder by using evidence-based guidelines, transferring the knowledge gained from the Texas Medication Algorithm Project (TMAP). This computerized decision support system (CompTMAP) provides support in diagnosis, treatment, follow-up, and preventive care and can be incorporated into the clinical setting. CompTMAP has gone through extensive testing to ensure accuracy and reliability. Physician surveys have indicated a positive response to CompTMAP, although the sample was insufficient for statistical testing. CompTMAP is part of a new era of comprehensive computerized decision support systems that take advantage of advances in automation and provide more complete clinical support to physicians in clinical practice.
Recent advances in medicine have greatly improved our capacity to treat major depressive disorder with drugs that are safer and more effective. The dramatic increase in new information and in the number of available antidepressants in the past decade have created a need to provide psychiatrists and primary care physicians with timely access to information about these new drugs (1,2). Because treatment guidelines can improve patient outcomes, methods for expanding the use of guidelines represent an important step in improving depression care. Extensive evidence has highlighted the difficulties encountered in implementing paper-and-pencil guidelines and algorithms. Fortunately, many studies have shown that these constraints can be overcome through the use of computerized systems, resulting in improved physician use and patient outcomes (3).
In 1999 health care experts from Europe and the United States met to confront the well-documented challenges to the implementation of guidelines and to identify strategies for improvement. They recommended a multifaceted approach to improving care—in particular, designing systems that facilitate change rather than attempting to impose change on physicians' behavior (4).
One approach is to design practice guidelines that can be incorporated into the workflow as an integral part of operations in the form of computerized decision support systems. A growing body of research indicates that physicians' use and adherence to guidelines are improved when the guidelines are furnished in a computerized format (5,6,7,8,9,10,11). Computerized decision support systems and computer information systems currently being used in medicine have indeed been associated with improved outcomes.
In recognition of the fact that optimal treatment of depression has been difficult to accomplish, we developed a computerized prompting and decision support system (12). In this article we briefly discuss methods previously used to enhance the use of evidence-based treatment and information technology in medical practice in general and illustrate our prototype for use by psychiatrists and primary care physicians in the treatment of depression.
Benefits of computerized decision support systems
In the following sections we discuss the benefits of some of the decision support systems designed to address specific areas of patient care.
Diagnosis
A recent study by Rollman and colleagues (13) examined the results of an electronic medical record (EMR) system in a primary care setting that provided electronic feedback to physicians in the diagnosis of depression. Primary care physicians who agreed with the diagnosis provided by the EMR feedback (65 percent of 186 physicians) were more likely to document the diagnosis of depression, to start the patient on antidepressant therapy, or to provide a referral to a mental health specialist. According to these authors, the EMR offered a way to disseminate current clinical practice guidelines and to direct the use of clinical practice guidelines by primary care physicians. However, in a later study, Rollman and associates (14) found that this EMR was not associated with improved patient outcomes.
Treatment decision support
Computerized decision support systems have been shown to be particularly useful for the purposes of prescribing medication, which is the most common intervention in medicine (15). This usefulness has been illustrated in studies showing improved anticoagulation therapy (16,17,18,19), improved antibiotic use and reduced adverse drug events (20,21,22), and improved dosing (7,23). For example, a meta-analysis of computer support by Walton and colleagues (23) showed a reduction in the time to reach therapeutic control (even when total drug use was unchanged) and a lower incidence of negative side effects when a computerized system was used.
Other benefits
Several studies have indicated that computerized decision support systems are useful in other aspects of health care delivery. These areas include follow-up and preventive care (24,25,26,27,28,29), computerized physician order entry and adverse drug events (30,31,32,33,34,35), and electronic documentation and information retrieval (36).
Comprehensive systems and guideline support
Most computerized decision support systems are unidecisional tools—for example, a system that guides the timing of diagnostic tests, such as Pap smears. Some of these tools do provide assistance with treatment decisions—for example, providing advice on medication use and preventive care. A computerized decision support system that is likely to enhance clinical care for depression must incorporate and include a majority of such aspects of care into one system, providing more complete support to physicians in practice.
Tierney and colleagues (10) have strongly suggested that computerized decision support systems should be designed to be comprehensive, not mere unidimensional tools. These authors state that guidelines need to account for comorbid conditions, concurrent drug therapy, the timing of most interventions, and follow-up. We developed a program that incorporates all the elements discussed above, because we recognized the importance of these elements (36,37).
CompTMAP
The computerized decision support system developed at the University of Texas Southwestern Medical Center, called CompTMAP (after the Texas Medication Algorithm Project guidelines and algorithms), is a computerized treatment algorithm for the treatment of depression and other psychiatric illnesses and is designed for use by both psychiatrists and primary care physicians. The TMAP was a large-scale study designed to determine the clinical and economic value of using medication algorithms in combination with clinical support and a patient-family educational package in the pharmacologic management of patients with one of three major mental disorders—schizophrenia, bipolar disorder, and major depressive disorder—each compared with treatment as usual in the public mental health sector (12).
Patients who were treated for major depressive disorder in the TMAP had better outcomes than those who received treatment as usual (12). However, problems related to dosage, visit duration, and visit frequency were identified. In general, dosages of selective serotonin reuptake inhibitors were in the range recommended by the algorithm, but oral dosages of the tricyclic antidepressants nefazodone, venlafaxine, and bupropion were lower than recommended by the algorithm. Visit frequency was less than recommended—the time between visits was close to three weeks rather than the one week recommended to ensure optimal dosage adjustments, symptom and side effect monitoring, patient education, and retention. Implementation of the algorithm was also accomplished with the help of a clinical coordinator at each of the clinics, which involved additional costs.
To address these key implementation issues, CompTMAP provides all the prompts necessary to implement the algorithm without the need for additional personnel, such as a clinical coordinator as required in the TMAP. The computerized algorithm makes it simple to follow the suggested dosage schedules and tactical recommendations by displaying the recommended dosage and treatment options for the appropriate week in treatment. All patient information, medication information, medication dosages, next appointments, and progress notes are recorded electronically and are readily accessible. Physicians using the program are given a recommended timeframe during which the patients return, which is based on the patient's stage in the algorithm. An advantage of CompTMAP is that feedback is ongoing and is available during clinic visits rather than only before or after the visits.
Features of CompTMAP
CompTMAP provides decision support in diagnosis, appropriate treatment choices, and follow-up and preventive care as well as access to physician order entry, alert systems, electronic documentation, and information retrieval.
Diagnosis
CompTMAP provides a list of major psychiatric diagnoses as categorized in DSM-IV, as can be seen in Figure 1. It also provides a link to the American Psychiatric Association practice guidelines that provide information about how to perform a diagnostic evaluation, although it does not provide an expert diagnostic system. The system does provide more than 15 measurement tools that can be used to help clinicians monitor symptoms and functional status over time.
Treatment decision support
The physician obtains clinical decision support by using CompTMAP to analyze pertinent information about the patient's current clinical condition that has been entered by the physician at each visit. The patient information is integrated with the rules of the program, which are based on expert knowledge. The required information necessary for the analysis is based on three aspects of the patient's current status: compliance, response to treatment in terms of symptoms and function, and the burden of side effects. Once this information is entered, the "rules engine" of the software is invoked.
The rules engine analyzes the new information about the patient that the physician has entered, along with several other pieces of information, such as how long the patient has been receiving the current treatment, the amount of time at that dosage, and blood concentrations of the medication, if applicable. After analyzing the information, CompTMAP offers the appropriate treatment options, including dosage options, an example of which can be seen in Figure 2. The program provides the physician with suggestions for treating with the primary and augmenting medications and also provides treatment choices for associated symptoms and side effects. Explanations and suggestions are provided in a decision support window on the same screen on which the treatment options are displayed (Figure 2).
To ensure physician autonomy, the physician can deviate from the recommendations at any time by clicking the physician override box and providing his or her rationale for overriding the recommendation. All possible options are then enabled, and the physician can make his or her selection.
Follow-up and preventive care
CompTMAP provides reminders to physicians through screen prompts to ensure that important considerations are not overlooked. For example, if a physician prescribes a mood stabilizer, such as lithium, or some other medication that requires close monitoring of blood drug concentrations, he or she is prompted to order blood tests for that medication. The program can also recommend and display the number of weeks in which the patient should return for a visit on the basis of the patient's status and stage in the algorithm.
Physician order entry and error prevention
The physician initially chooses the psychotropic medications and dosages from pull-down menus on the treatment selection screen (Figure 2). The selected medications then appear on the prescription screen along with the suggested route and frequency of administration. The physician can choose to adjust the frequency and type by writing specific instructions in the comments section. A prescription can be generated.
Adverse drug event alert systems
When medication errors are made, CompTMAP displays a warning box. For example, if a physician tries to order two benzodiazepines, the physician is notified that he or she has ordered two medications from the same family of medications. For medications that require blood monitoring before the dosage can safely be increased, the physician is notified that a blood reading is necessary. If a physician tries to order two medications that should not be administered together or that require caution if they are administered together, the physician is notified of the potential problem.
Documentation, record keeping, and information retrieval
All entries are automatically stored, providing electronic documentation and record keeping. Thus the physician has ready access to complete patient information. Clinical status and prescription history are presented in easy-to-read graphs for each visit, as can be seen in Figure 3. Additional information, such as patients' demographic characteristics, blood drug concentrations, symptom rating scale scores, and complete progress notes, is also accessible by clicking on the toolbar at the top of the screen in any section of the application.
Automatic physician notes are created and recorded as a by-product of the physician's actions during a visit without the need for the physician to type any information. Additional notes can be written as necessary. The patient's progress is recorded throughout the course of care as progress notes and is also displayed graphically to show severity of symptoms, functional status, and side effect burden over time (Figure 3). The medication choices are also recorded in the progress notes, under prescription history, and graphically. The patient's demographic characteristics, history, physician ratings, mental status examination results, symptom scale scores, and blood drug concentrations are a part of the record. A pull-down list of CPT codes and billing processing is also available to assist in billing.
The program can be integrated into currently used clinic systems, can be interfaced to another computer application, can be used to import and export data and files, can provide online access to a main database, and can link to useful Web sites.
CompTMAP testing and physician use
CompTMAP has gone through extensive testing to ensure accuracy and reliability. Phase 1 of testing began after the computer programmers, under the guidance of the project development team, had finished entering the initial data and rules into the application and released the introductory version. This phase included testing of the program by all the professionals who worked on the project.
Phase 2 of testing involved a three-step process. Phase 2A testers were first introduced to the application and trained on its use. This select group comprised physicians and pharmacists who were considered experts in their fields and in the TMAP algorithms. The group was asked to create "test" patients, whom they entered at various stages of the algorithm and at different critical decision points in the stage with various assessments of response, adherence to medications, and side effect burden. Phase 2B involved entering actual patient chart data into CompTMAP. TMAP data were entered for 80 patients, as were chart data for 80 currently active patients in two different centers of the Texas Department of Mental Health and Mental Retardation.
Phase 2C, the initial field-testing of CompTMAP, involved implementation of the program at two Texas public health sector sites. The first test included three psychiatrists who conducted an extended review of CompTMAP on three laptop computers. After they had been trained, these psychiatrists were allowed to use the system for two to three weeks with their patients. The second test included four psychiatrists in a field trial (at the second site). The second group then used CompTMAP with patients for four to six weeks. All seven psychiatrists were asked to complete an ease-of-use survey and a usefulness survey (38). The psychiatrists in the field trial group reported using the software with ten to 14 patients each and for about two to four hours per week.
The Ease of Use Survey (38) consists of 12 items that can be summarized as three scores: a global impression (one item: How easy was the software program to use?), software ergonomics (six items—for example, How easy was it for you to find what you were looking for on the screen? and How easy is it to correct mistakes?), and visit mechanics (five items—for example, How easy was the software program to use in the presence of patients? and How easy was the software program to use with your daily workflow?). All items were rated on 7-point scales, with 1 indicating not at all easy to use and 7 indicating very easy to use.
The 13 items of the Usefulness Survey (38) can also be summarized as three scores: a global impression (one item: Overall, how useful was the software program?), treatment information (five items—for example, Did you find the treatment recommendation useful?), and visit duties (seven items—for example, How useful was the software in the prescribing of medication?). All items were rated on 7-point scales, with 1 indicating not useful at all to 7 indicating very useful.
The results of the surveys are presented in Table 1 for both the extended review and the field trial. Although this sample was insufficient for statistical tests, all ratings were above the midpoint on the scales, indicating a positive response to CompTMAP. In general, the responses related to longer-term use (the field trial sample) were better than those related to shorter-term use (the extended review).
Conclusions
Although extensive evidence has highlighted the difficulties encountered in implementing paper-and-pencil practice guidelines and algorithms, many studies have shown that computerized systems have the potential to overcome these constraints, resulting in improved physician use and patient outcomes (3). Depression guidelines provided in a comprehensive computerized format that can be integrated into psychiatric and primary care settings can remain a part of the process of care.
We plan to implement the computerized system in the primary care setting and in the public sector to determine factors such as the time it takes to use the system, workflow issues, accessibility issues, and patient response and outcomes. These questions are being evaluated in subsequent studies, including our ongoing effectiveness trial. We acknowledge that there are barriers to acceptance beyond a computer system's ability to be integrated into a complex organizational environment; a main barrier is physician acceptance. Barriers to acceptance of computerized programs by physicians can include physicians' knowledge of and attitudes toward computers in general. However, time constraints and the real-world usability of the program also play a role. Accordingly, recommendations from physicians who have used the program in clinical settings have been and will continue to be incorporated into the program.
CompTMAP is part of a new era of comprehensive computerized decision support systems that take advantage of advances in automation, providing more complete clinical support to physicians in clinical practice. Such advances hold the promise of enhancing quality of care for depression. These comprehensive tools have the potential to simplify and improve record keeping and to bring the most current medical treatment research to physicians in a form that they can use in their practice.
Acknowledgments
This research was funded in part through grant RO1-MH-06406201A2 (MHT) from the National Institute of Mental Health. The authors acknowledge the support of Mental Health Connections, a partnership between Dallas County Mental Health and Mental Retardation (MHMR); the department of psychiatry of the University of Texas Southwestern Medical Center at Dallas, which receives funding from the Texas State Legislature and the Dallas County Hospital District; and the National Alliance for Research in Schizophrenia and Depression (MHT). The authors also thank the members of the CompTMAP team at Clinical Information Services: Preston Park, B.S., M.C.S.D., Michael Goodloe, M.B.A., Anne McClelland, B.S., Elizabeth Schindler, B.B.S., Hua Liang, Ph.D., Shan Sheely, B.S., Jenny Liou, B.S., Jin Fan, M.D., Jimmy Bryant, B.S., and Jay Marrow, D.V.M.
The authors are affiliated with the department of psychiatry of the University of Texas Southwestern Medical Center, 5323 Harry Hines Boulevard, Dallas, Texas 75390-9119 (e-mail, [email protected]).
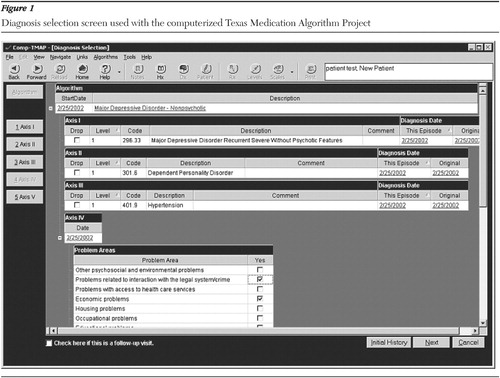
Figure 1. Diagnosis selection screen used with the computerized Texas Medication Algorithm Project
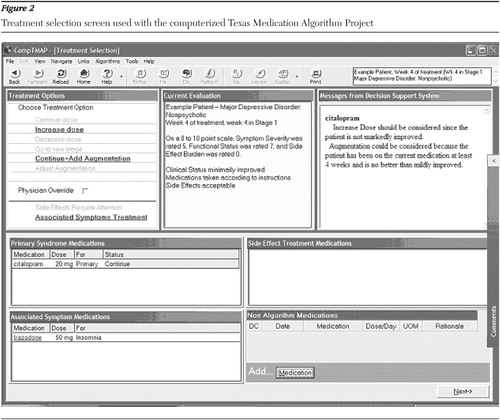
Figure 2. Treatment selection screen used with the computerized Texas Medication Algorithm Project
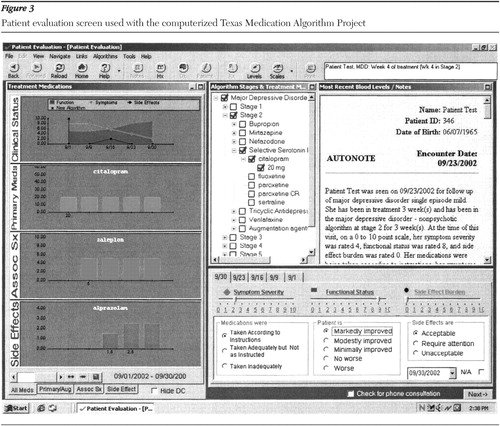
Figure 3. Patient evaluation screen used with the computerized Texas Medication Algorithm Project
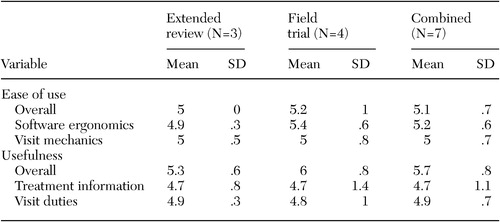 |
Table 1. Results of a physician survey on the ease of use and usefulness of the computerized Texas Medication Algorithm Project (CompTMAP) system in clinical care
1. Galvin PM, Knezek LD, Rush AJ, et al: Clinical and economic impact of newer versus older antipsychotic medications in a community health center. Clinical Therapeutics 21:1105–1116, 1999Crossref, Medline, Google Scholar
2. Casey D: The relationship of pharmacology to side effects. Journal of Clinical Psychiatry 58:55–62, 1997Medline, Google Scholar
3. Elson RB, Connelly DP: Computerized patient records in primary care: their role in mediating guideline-driven physician behavior change. Archives of Family Medicine 4:698–705, 1995Crossref, Medline, Google Scholar
4. Gross PA: Implementing evidence-based recommendations for health care: roundtable comparing European and American experiences. Joint Commission Journal on Quality Improvement 26:547–553, 2000Crossref, Medline, Google Scholar
5. Anderson JD: Increasing the acceptance of clinical information systems. MD Computing 16:62–65, 1999Medline, Google Scholar
6. Greco PJ, Eisenberg JM: Changing physicians' practices. New England Journal of Medicine 320:1271–1274, 1993Crossref, Google Scholar
7. Hunt DL, Haynes BH, Hanna SE, et al: Effects of computer-based clinical decision support systems of physician performance and patient outcomes. JAMA 280:1339–1346, 1998Crossref, Medline, Google Scholar
8. Ebell MH, Hale W, Buchanan JE, et al: Hand-held computers for family physicians. Journal of Family Practice 41:385–392, 1995Medline, Google Scholar
9. Avorn J, Soumerai SB: Use of computer-based Medicaid drug data to analyze and correct inappropriate medication use. Journal of Medical Systems 6:377–386, 1982Crossref, Medline, Google Scholar
10. Tierney WM, Overhage JM, Takesue BY, et al: Computerizing guidelines to improve care and patient outcomes: the example of heart failure. Journal of the American Medical Informatics Association 2:316–322, 1995Crossref, Medline, Google Scholar
11. Linnarsson R: Decision support for drug prescription integrated with computer-based patient records in primary care. Medical Informatics (London) 18:131–142, 1993Crossref, Medline, Google Scholar
12. Trivedi MH, Rush AJ, Crismon ML, et al: Texas Medication Algorithm Project (TMAP): clinical results for patients with major depressive disorder. Archives of General Psychiatry 61:669–680, 2004Crossref, Medline, Google Scholar
13. Rollman BL, Hanusa BH, Gilbert T, et al: The electronic medical record: a randomized trial of its impact on primary care physicians' initial management of major depression. Archives of Internal Medicine 161:189–197, 2001Crossref, Medline, Google Scholar
14. Rollman BL, Hanusa BH, Lowe HJ, et al: A randomized trial using computerized decision support to improve treatment of major depression in primary care. Journal of General Internal Medicine 17:493–503, 2002Crossref, Medline, Google Scholar
15. Classen DC, Pestotnik SL, Evans S, et al: Adverse drug events in hospital patients. JAMA 279:301–306, 1997Crossref, Google Scholar
16. Fitzmaurice DA, Hobbs FD, Delaney BC, et al: Review of computerized decision support systems for anticoagulation management. British Journal of Haematology 102:907–909, 1998Crossref, Medline, Google Scholar
17. Chantellier G, Columbet I, Degoulet P: Computer-adjusted dosage of anticoagulant therapy improves the quality of anticoagulation. Medical Informatics (London) 9:819–823, 1998Google Scholar
18. Poller L, Shiach CR, MacCallum PK, et al: Multicentre randomised study of computerised anticoagulant dosage: European Concerted Action on Anticoagulation. Lancet 352:1505–1509, 1998Crossref, Medline, Google Scholar
19. Vadher BD, Patterson DL, Leaning M: Comparison of oral anticoagulant control by a nurse practitioner using a computer decision-support system with that by clinicians. Clinical and Laboratory Haematology 19:203–207, 1997Crossref, Medline, Google Scholar
20. Pestotnik SL, Classen DC, Evans RS, et al: Implementing antibiotic practice guidelines through computer-assisted decision support: clinical and financial outcomes. Annals of Internal Medicine 124:884–890, 1996Crossref, Medline, Google Scholar
21. Evans RS, Pestotnik SL, Classen DC, et al: A computer-assisted management program for antibiotics and other anti-infective agents. New England Journal of Medicine 338:232–238, 1998Crossref, Medline, Google Scholar
22. Shojania KG, Yokoe D, Platt R, et al: Reducing vancomycin use utilizing a computer guideline. JAMA 5:554–562, 1998Google Scholar
23. Walton R, Dovey S, Harvey E, et al: Computer support for determining drug dose: systematic review and meta-analysis. British Medical Journal 318:984–990, 1999Crossref, Medline, Google Scholar
24. Johnston ME, Langston KB, Haynes RB, et al: Effects of computer-based decision support systems on clinician performance and patient outcome. Annals of Internal Medicine 120:135–142, 1994Crossref, Medline, Google Scholar
25. Sullivan F, Mitchell E: Has practitioner computing made a difference to patient care? A systematic review of published reports. British Medical Journal 311:848–852, 1995Crossref, Medline, Google Scholar
26. Chambers CV, Valban DJ, Lepidus CB, et al: Microcomputer-generated reminders: improving the adherence of primary care physicians with mammography screening guidelines. Journal of Family Practice 29:273–280, 1989Medline, Google Scholar
27. Tierney WM, Hui SL, McDonald CJ: Delayed feedback of physician performance versus immediate reminders to perform preventive care. Medical Care 24:659–666, 1986Crossref, Medline, Google Scholar
28. Tape TG, Campbell JR: Computerized medical records and preventive care: success depends on many factors. American Journal of Medicine 94:619–625, 1993Crossref, Medline, Google Scholar
29. Litzelman DK, Dittas RS, Miller ME, et al: Requiring physicians to respond to computerized reminders improves their adherence with preventative care protocols. Journal of Internal Medicine 311–317, 1993Google Scholar
30. Bates DW, Leape LL, Cullen DJ, et al: Effect of computerized physician order entry on prevention of serious medication errors. JAMA 280:1311–1316, 1998Crossref, Medline, Google Scholar
31. Bates DW, Teich JM, Lee J, et al: The impact of computerized physician order entry on medication error prevention. Journal of the American Medical Informatics Association 6:313–321, 1999Crossref, Medline, Google Scholar
32. Tierney WM, Miller ME, Overhage JM, et al: Physician inpatient order writing on microcomputer workstations: effects on resource utilization. JAMA 269:379–383, 1993Crossref, Medline, Google Scholar
33. Raschke RA, Gollihare B, Wunderlich TA, et al: A computer alert system to prevent injury from adverse events. JAMA 280:1317–1320, 1998Crossref, Medline, Google Scholar
34. Understanding and preventing drug misadventures: a multidisciplinary invitational conference sponsored by the ASHP Research and Education Foundation in cooperation with the American Medical Association, the American Nurses Association, and the American Society of Hospital Pharmacists. American Journal of Health-System Pharmacy 52:369–416, 1995Medline, Google Scholar
35. Kohn LT, Corrigan JM, Donaldson MS: To err is human: building a safer health system. Committee on Quality Health Care in America, Institute of Medicine. November, 1999. Available at http://books.nap.edu/html/to_err_is_human/exec_summ.html. Accessed May 1, 2001Google Scholar
36. Trivedi MH, Kern JK, Baker SM, et al: Computerized medication algorithms and decision support systems in major psychiatric disorders. Journal of Psychiatric Practice 6:237–246, 2000Crossref, Medline, Google Scholar
37. Trivedi MH, Kern JK, Voegle T, et al: Computerized medical algorithms in behavioral health care, in Behavioral Health Care Informatics. Edited by Dewan NA, Lorenzi N, Riley R, Bhattacharya SR. New York, Springer-Verlag, 2001Google Scholar
38. Trivedi MH, Kern JK, Marcee AK, et al: Development and implementation of computerized clinical guidelines: barriers and solutions. Methods of Information in Medicine 41:435–442, 2002Crossref, Medline, Google Scholar



