The Partners in Care Approach to Ethics Outcomes in Quality Improvement Programs for Depression
Abstract
OBJECTIVE: Patient centeredness and equity are major quality goals, but little is known about how these goals are affected by efforts to improve the quality of care. The authors describe an approach to addressing these goals in a randomized trial of quality improvement for depressed primary care patients. METHODS: For four ethics goals (autonomy, distributive justice, beneficence, and avoiding harm), the authors identify intervention features, study measures, and hypotheses implemented in Partners in Care, a randomized trial of two quality improvement interventions, relative to usual care and summarize published findings pertinent to these outcomes. RESULTS: To implement an ethics framework, modifications were required in study design and in measures and analysis plans, particularly to address the autonomy and justice goals. Extra resources were needed for sample recruitment, for intervention and survey materials, and to fund an ethics coinvestigator. The interventions were associated with improvements in all four ethics areas. Patients who received the interventions were significantly more likely to receive the treatment they had indicated at baseline as their preferred treatment (autonomy goal). Intervention-associated benefits occurred more rapidly among sicker patients and extended to patients from ethnic minority groups, resulting in a reduction in ethnic-group disparities in health outcomes relative to usual care (distributive justice goal). The interventions were associated with improved quality of care and health outcomes (beneficence goal) and with reduced use of long-term minor tranquilizers (goal of avoiding harm). CONCLUSIONS: It is feasible to explicitly address ethics outcomes in quality improvement programs for depression, but substantial marginal resources may be required. Nevertheless, interventions so modified can increase a practice's ability to realize ethics goals.
The formulation of quality-of-care goals in medicine has expanded to include values such as patient centeredness (1). National data suggest that care for most medical conditions meets accepted standards for technical quality for only about half of patients (2). The prevailing approach to this problem is quality improvement programs, such as the collaborative approach to chronic disease management (3,4). Quality improvement programs have been evaluated for many conditions, including depression (5,6,7,8,9,10,11,12). In primary care, depression serves as an excellent tracer for studying quality problems, because although it can be treated effectively and involves high social costs, it is often undetected and untreated in primary care settings (13,14,15,16,17). Quality improvement programs for depression can improve quality of care and health outcomes for two years and beyond (5,6,7,8,9,10,11,12). However, few studies have evaluated the effects of quality improvement on ethics goals (18,19,20).
In this article we address this gap by illustrating how four ethics goals can be incorporated as outcomes in demonstrations of quality improvement, using depression in primary care as an example (21,22,23,24,25,26,27). Two ethics goals—beneficence and avoiding harm—are fundamental to quality improvement and might not seem to require separate attention. However, aspects of these goals fall outside the utilitarian framework that guides most quality improvement efforts and merit separate attention under a broader perspective. Patient autonomy and distributive justice are our major focus and have rarely been included as goals in quality improvement evaluations. Yet leaders in health policy and public interest groups have emphasized the importance of addressing client centeredness (one aspect of autonomy) and equity (one aspect of distributive justice) as quality goals (1,17,28,29).
The Institute of Medicine and others have noted that promoting autonomy can compete with promoting equity, so special care is needed when addressing both goals in quality improvement (1,30). Here we address such issues by reviewing how Partners in Care (PIC) (31), a Patient Outcomes Research Team II (PORT-II) project of the Agency for Healthcare Research and Quality, adopted an ethics framework. We review the PIC study design and, for each of four ethics goals, discuss the framework that informed the study and how we modified the design and measures, and we summarize our hypotheses and relevant published findings.
Methods
Design of Partners in Care
PIC is a group-level randomized trial of the effects of quality improvement programs for depressed patients in primary care on cost, health outcomes, and quality of care (31,32,33). Seven managed primary care group practice organizations were recruited, selected to produce a practice sample that was diverse in organization and location and a patient sample that was overrepresentative of Latino persons, particularly Mexican Americans, while including African Americans at each site.
Across organizations, 46 matched primary care clinics were randomly assigned to provide either care as usual or one of two quality improvement interventions. A total of 181 primary care providers were enrolled. In each clinic, a consecutive patient sample was screened for depression with use of a self-report depressive symptom measure followed by a standard diagnostic interview. A total of 1,356 ongoing care patients with depression who had eligible insurance (that is, insurance or a public program that would potentially reimburse for services from intervention providers) were enrolled between June 1996 and April 1997. Participating patients were asked to complete baseline and semiannual follow-up surveys and interviews over two years and at 57 months.
Two quality improvement interventions were developed—one involving medications and the other involving therapy. The interventions provided information and resources for obtaining appropriate care for depression— either antidepressant medication or psychotherapy—without assigning or requiring treatment. Each intervention included four components: commitment of in-kind resources from the practices to support quality improvement; local clinician teams (consisting of a mental health specialist, a primary care clinician, a nurse, and in some practices an administrator) trained by study investigators to implement quality improvement strategies and to adapt them to local practice priorities and resources; a toolkit of clinician and patient education materials; and trained depression nurse specialists to educate, assess, and activate patients and facilitate initial treatment—that is, medication management or referral to therapy if indicated. In addition, each intervention had supplemental resources.
The resources for the medication intervention consisted of an extension of the nurse specialist role to provide follow-up on compliance with psychotropic medications for six or 12 months. The resources for the therapy intervention consisted of a reduction in copayment for up to 12 sessions of therapy from a practice therapist who was trained by the study in individual and group cognitive-behavioral therapy and was also trained to communicate regularly with the primary care provider (31,32,33).
Ethics consultation
The study funded an ethics coinvestigator (the first author, at 10 to 20 percent for three years) to educate investigators, consult about conflicts inherent in resource allocation, and observe project planning meetings to identify and help resolve ethical concerns. The coinvestigator identified opportunities for measuring ethics outcomes, participated in pretesting activities to observe consumers' reactions to study materials, and presented the overall ethics perspective and goals to practice representatives at the first advisory board before the study was implemented. The consultation benefited from existing literature on ethical issues in the development of practice guidelines (23,24,25). The ethicist on this study was a psychiatrist and ethicist who had also trained in health services research. The study was approved by the institutional review boards of RAND and the participating practices and institutions.
Results
The four ethics goals, the intervention and study design modifications, and key hypotheses are outlined in Table 1. Ethics outcome measures and summaries of published findings are shown in Table 2. Below we briefly describe the study framework and highlight key points from the two tables.
Autonomy and respect for persons
The concept of autonomy, or self-rule, is often applied narrowly in medicine to a single encounter in which a patient gives adequately informed consent—or refusal—free from paternalistic interference. This emphasis on noninterference ignores the advocacy efforts by providers that may be needed to ensure exercise of autonomy by populations whose self-advocacy is limited—for example, because of cognitive deficits during depression. Furthermore, a broader conception of respect for autonomy is needed to respond to patients' needs, not only the need to give informed consent at one moment in time but also the need to receive types of treatment that promote their own life goals over time (34,35).
We approached autonomy from a systems perspective. Patients' options depend on physicians' knowledge and attitudes, and findings from focus groups suggested that some managed care physicians tended not to offer psychotherapy, because they perceived it as less effective and less accessible than medication. We therefore thought that optimal practice culture should educate both physicians and patients to support alternative, effective treatments (different evidence-based medications and psychotherapies) and ongoing access to information about their costs and benefits.
Interventions. The interventions for the autonomy goal were designed to facilitate informed choice and genuine treatment options over time for patients and clinicians: patients and clinicians had full choice over treatment (including the option of no treatment), and practices could modify the interventions to fit their priorities and resources. The nurse specialists, through their communication activities and education toolkits for patients, enabled informed choice over time. Clinician training materials also encouraged attention to patients' preferences (Table 1).
Study design and measures. The interventions randomly assigned clinics to information and resources that encouraged appropriate care rather than to treatments. To measure patients' treatment preferences and patients' and providers' knowledge, survey items were added at baseline and at six-month patient follow-up and 18-month provider follow-up.
Hypotheses and findings. We hypothesized that the interventions would improve patients' and providers' knowledge about treatment and increase the proportion of patients receiving the treatment that they initially preferred (Table 1). The intervention involving therapy was associated with a significant increase in patients' knowledge (t=2, df=998, p=.05; a similar trend was observed for the pooled interventions (p=.056). (These are previously unreported results.) In addition, the results showed that the combined quality improvement interventions improved clinicians' knowledge about counseling and tended to improve overall knowledge (36). Furthermore, the interventions increased the proportion of patients at six and 12 months who received the treatment that they had preferred at baseline, relative to the patients who received usual care (37).
Distributive justice
Our working assumption was that explicit attention to justice is needed in designing quality improvement interventions, because individuals from underserved ethnic minority groups are likely to face ongoing societal barriers when attempting to obtain better care. Furthermore, interventions based on practice guidelines that have been formulated for the average patient may lead to insufficient attention being given to the particular needs of the sickest or more complex patients, such as those with suicidal ideation.
PIC's approach to the distributive justice goal was influenced by the work of Rawls (38). From this perspective, it is unfair to allow people to be saddled with disadvantages that are not the result of their own choices and that prevent them from meeting their basic needs when such an outcome is preventable. Thus far, thinkers such as Daniels (39) have applied Rawlsian ideas to health care by using a definition of need based on severity of illness and functional limitations. We expand this conception to include a focus on disparities that reflect historical and current disadvantage (17,40).
Intervention. Practice administrators were encouraged to develop methods to facilitate access, particularly to psychotherapy, among patients from ethnic minority groups. When available, quality improvement components were selected that had been evaluated among low-income minority patients—for example, cognitive-behavioral therapy (41,42). Examples of modifications made by the practices include increasing the number of bilingual nurses or therapists, having therapy sessions in primary care settings, or conducting therapy by telephone. The expert leader, intervention staff, and clinician training materials included suggestions for addressing needs of sicker and more complex patients. The therapy intervention included a form of cognitive-behavioral therapy (four sessions) that was tailored to patients with minor depression. Practice therapists preferred having something to offer such patients. This modification was based on evidence that cognitive-behavioral therapy in minor depression may reduce symptoms of depression (43) and that individual components of cognitive-behavioral therapy may be as effective as full cognitive-behavioral therapy (44).
Study design and measures. PIC included a large number of Latino persons (primarily Mexican Americans), who constituted about a third of the sample, and included one public-sector organization with uninsured patients. The costs of modifying study materials for Spanish-speaking patients were equivalent to about half the (marginal) implementation costs of adding one site to the study, or $100,000. All surveys were field tested in Spanish and English, type fonts were enlarged for elderly patients, telephone assistance was available, and patients with hearing or other impairments could participate through in-person interviews in a location of their choice. The study included patients who at baseline had had current depressive symptoms and depressive disorder within the previous 12 months as well as those who had had current depressive symptoms without disorder within the previous 12 months. These patients were included to determine how practices prioritized the care of sicker patients and because the interventions were designed to facilitate management of a group of patients who were at high risk of developing depressive disorder, which included tracking patients who had symptoms only to watch for early evidence of disorder and to initiate treatment. No special measures were necessary to examine these outcomes.
Hypotheses and findings. We formulated three hypotheses about equity goals, which are listed in Table 1. First, we hypothesized that the benefits of quality improvement, in terms of improved quality of care and outcomes, would extend to and include Latinos and African Americans. We found that quality of care improved in all ethnic groups, with a greater gain in clinical outcomes in the first follow-up year under quality improvement for these minority groups relative to white persons. Benefits in the area of employment were significant among whites; a similar trend was found among the minority groups, but the statistical power to detect this effect was low, and the finding was not significant (45).
The second hypothesis was that the interventions would reduce disparities in health outcomes between white patients and patients from ethnic minority groups (17). We found that under usual care, African-American and Latino persons had worse outcomes than white persons in the first year but that this disparity was reduced for participants in clinics with the quality improvement initiatives (45).
Our third hypothesis was that the quality improvement interventions would be associated with greater improvements in quality of care among sicker patients who initially had depressive disorder than among patients who had only depressive symptoms. We found that in the first six months, the effects of the intervention on quality of care and health outcomes were stronger among patients who had had depressive disorder for the previous year at baseline than among those who had depressive symptoms without disorder. However, by the 12-month follow-up, the effects associated with the quality improvement interventions were comparable. Thus sicker patients initially were given higher priority for treatments. After the first six months, more equal outcome effects by baseline disorder status could reflect greater initial improvement among persons with a disorder and progression to a disorder among some of the patients who initially had only symptoms.
Beneficence
Beneficence refers to the positive duty of fiduciaries to benefit each person whom they are entrusted to serve and to the utilitarian goal of optimizing outcomes for a population (46). The former use of beneficence reflects an individual client perspective that may resonate with practice goals of individual clinicians but that is easy to overlook when such programs are implemented in the context of practice strategies to contain rising costs. In this respect, the latter use of beneficence in reference populations is likely to be the perspective that guides outcome goals related to quality improvement at the practice administrator level. The study focused on improving average outcomes while expanding benefits to specific vulnerable populations but respected the right of practices to serve patients according to their cultural norms and resources. From an ethics perspective, this approach represents a compromise. However, it facilitated a separate scientific study goal of evaluating the impact of quality improvement interventions as naturalistically implemented by practices.
Interventions. For the beneficence goal, the interventions provided information and resources to facilitate the recognition and assessment of depression and to increase appropriate treatment (31,32).
Hypotheses and findings. As we hypothesized, the interventions were associated with improvements in quality of care and mental-health-related outcomes and with an increase in the proportion of patients who were employed (33). Improved health outcomes persisted into the second follow-up year for patients in the therapy intervention, and benefits in the area of employment continued into the second year for both interventions. Higher use of antidepressant medication continued into the second follow-up year for patients who received the medication intervention (47,48,49,50).
Avoiding harm
Nonmaleficence is neither absolute nor independent of beneficence. Many medical procedures involve minor harm in producing larger benefits. Furthermore, interventions that aim to maximize cost-effectiveness may conflict with interventions that seek to protect each individual patient from harm. We did not face this conflict in PIC, because our interventions sought to reduce harm by reducing the use of minor tranquilizers in the absence of comorbid anxiety, and this was also expected to improve cost-effectiveness (5,15).
Intervention features. Our quality improvement manual for clinicians specifically recommended avoidance of long-term minor tranquilizers in the absence of comorbid anxiety disorder. In the medication intervention, the nurse specialist reinforced this recommendation through follow-up (Table 2).
Study design and measures. No special modifications were necessary other than collecting information about the long-term use of minor tranquilizers in each follow-up survey and assessing comorbid anxiety at baseline.
Hypothesis and findings. As we hypothesized, the medication intervention tended to be associated with lower use of long-term minor tranquilizers, especially at two years, compared with the therapy intervention and usual care (49).
Discussion
We found that it was feasible to adopt a standard ethics framework for developing practice guidelines for application in a major demonstration of quality improvement for depression in primary care. Adopting this framework required modification of the interventions, study design, and measures. We formulated new hypotheses and analysis plans to address the less commonly studied domains of autonomy and distributive justice. Our model for these modifications may serve as a template for other evaluations of quality improvement programs. Our empirical findings suggest that these modifications permit practices to more fully realize these ethics goals. For example, we found that this type of quality improvement intervention was associated with an increase in the percentage of patients who received their most preferred treatment among reasonable alternatives and with reductions in preexisting disparities in health outcomes by benefiting Latino and African-American persons in particular. Documenting such achievements could have other benefits for practices, such as increasing enrollment.
Addressing these ethics goals—particularly autonomy and distributive justice—and integrating them fully with the scientific goals of the project required substantial modifications to the study and substantial resources to be set aside. One key innovation was random assignment of opportunities for care rather than treatment per se. This approach enabled us to evaluate the impact of the interventions on realization of patients' preferences. The sample size that was required to enable observation of the intervention effect—given that "encouragement" rather than treatment was randomized—was large (N= 1,356). These design modifications were also necessary to address another study goal of estimating, through observational analyses, the effectiveness of treatments for depression under naturalistic care conditions (51).
The realization that this design afforded a unique opportunity to examine implications of quality improvement for patients who were being offered genuine options and then receiving preferred care—aspects of autonomy—is one example of the benefits of proactive ethics collaboration. Furthermore, the study identified patients through routine screening of visitors to the practices rather than the more common approach of clinician referral. This approach was selected to increase the generalizability of findings to consecutive patients visiting these practices and to reduce unobserved sources of heterogeneity due to provider referral criteria. However, it also represented an opportunity to optimize beneficence among patients whose depression was not already detected by their provider.
The inclusion of a large sample of patients from ethnic minority groups and modifications for Spanish-speaking patients derived more exclusively from an ethics (justice) objective, and study modification costs were substantial (we think at least $100,000). Implementing the more conventional ethics goals of beneficence and avoiding harm only trivially increased study costs. Formulating and implementing the full framework required three years of funding for an ethics coinvestigator, not the usual few days of consultation. In addition, it was necessary to work collaboratively with the practices to discuss the value of addressing these goals in the study design phase.
The PIC ethical framework, as implemented, had some important limitations. The intervention methods did not include an explicit method, such as a computerized decision analysis tool, to inform and address diverse values of patients or clinicians. Although others have been developing computerized decision aides on the basis of guidelines for depression care (52)—and these decision support tools can incorporate information about patients' values—few actually do so. Such developments seem to represent an important and feasible direction for future quality improvement programs. In addition, our measures of ethics outcomes were self-reported by patients or providers.
Furthermore, as noted above, the study's approach to beneficence represented a compromise from an ethics standpoint in that it promoted quality while respecting the practices' organizational values and resource constraints. Such a position means that conflicts between the value of an individual patient's needs and a plan's resources can remain unresolved. However, it also represents a form of "neutrality" that permits the real stakeholders to reveal their priorities through the study data and findings while facilitating the study goal of observing practice-directed implementation of quality improvement. Thus the patients, providers, and practices themselves achieved the ethics outcomes reported by the study.
Conclusions
In conclusion, it is feasible to explicitly incorporate ethics goals into quality improvement demonstrations fielded in community practices. Furthermore, such programs can contribute to substantial, measurable improvements in ethics goals in the care of depressed patients. Although incorporating an ethics perspective entails real costs, the interventions achieved cost-effectiveness ratios in the range of widely used medical therapies (53). Thus it is possible to approach clinical, economic, and ethics goals of health care through programs that encourage use of guideline-concordant care by providing education and resources to enable flexible choice of treatment while encouraging inclusion of diverse populations. However, the impetus for substantial commitment to autonomy, justice, and other ethics domains as outcomes of quality improvement programs ultimately depends on how important such goals are to patients, providers, and policy makers. By sharing our approach, we hope to increase debate on the value of this commitment.
Acknowledgments
This work was funded by the National Institute of Mental Health (grants P30-MH-068639, R01-MH-61570, and K12-MH-00990) and by the Agency for Healthcare Research and Quality (R01-HS08349). The authors thank Cathy Sherbourne, Ph.D., for contributing the new analyses on the impact of the interventions on patients' knowledge and Bernadette Benjamin, M.S., for excellent programming support.
Dr. Halpern is affiliated with the division of community health and human development of the School of Public Health at the University of California, Berkeley. Dr. Johnson was with the department of psychiatry at the University of Southern California in Los Angeles and is now with the department of psychiatry at the University of Washington in Seattle. Dr. Miranda is with the Neuropsychiatric Institute of the University of California, Los Angeles. Dr. Wells is with RAND in Santa Monica, California, and the Neuropsychiatric Institute of the University of California, Los Angeles. Send correspondence to Dr. Wells at RAND, 1700 Main Street, Santa Monica, California 90407-2138 (e-mail, kwells@ ucla.edu).
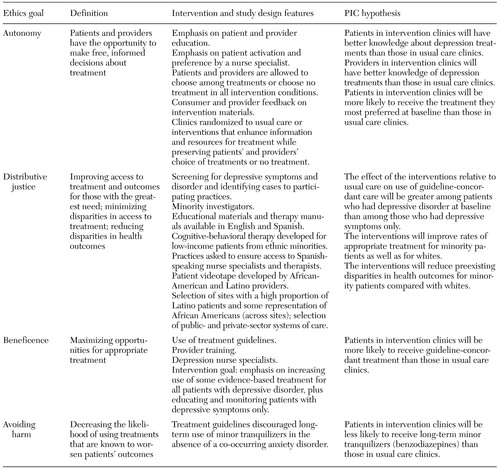 |
Table 1. Goal definitions, interventions and study design modifications, and Partners in Care (PIC) hypotheses for ethics outcomes
 |
Table 2. Partners in Care (PIC) measures and findings for ethics outcomes
1. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC, Institute of Medicine, Committee on Quality of Health Care in America, 2001Google Scholar
2. McGlynn EA, Asch SM, Adams J, et al: The quality of health care delivered to adults in the United States. New England Journal of Medicine 348:2635–2645, 2003Crossref, Medline, Google Scholar
3. Von Korff M, Gruman J, Schaefer J, et al: Collaborative management of chronic illness. Annals of Internal Medicine 127:1097–1102, 1997Crossref, Medline, Google Scholar
4. Wagner EH, Austin BT, Von Korff M: Organizing care for patients with chronic illness. Milbank Quarterly 74:511–544, 1996Crossref, Medline, Google Scholar
5. Katon W, Von Korff M, Lin E, et al: Collaborative management to achieve treatment guidelines: impact on depression in primary care. JAMA 273:1026–1031, 1995Crossref, Medline, Google Scholar
6. Katon W, Robinson P, Von Korff M, et al: A multifaceted intervention to improve treatment of depression in primary care. Archives of General Psychiatry 53:924–932, 1996Crossref, Medline, Google Scholar
7. Simon GE, Manning WG, Katzelnick DJ, et al: Cost-effectiveness of systematic depression treatment for high utilizers of general medical care. Archives of General Psychiatry 58:181–187, 2001Crossref, Medline, Google Scholar
8. Hunkeler EM, Meresman JF, Hargreaves WA, et al: Efficacy of nurse telehealth care and peer support in augmenting treatment of depression in primary care. Archives of Family Medicine 9:700–708, 2000Crossref, Medline, Google Scholar
9. Rost K, Nutting P, Smith J, et al: Improving depression outcomes in community primary care practice: a randomized trial of the quEST intervention: Quality Enhancement by Strategic Teaming. Journal of General Internal Medicine 16:143–149, 2001Crossref, Medline, Google Scholar
10. Von Korff M, Katon W, Bush T, et al: Treatment costs, cost offset, and cost-effectiveness of collaborative management of depression. Psychosomatic Medicine 60:143–149, 1998Crossref, Medline, Google Scholar
11. Katon W, Russo J, Von Korff M, et al: Long-term effects of a collaborative care intervention in persistently depressed primary care patients. Journal of General Internal Medicine 17:741–748, 2002Crossref, Medline, Google Scholar
12. Rost K, Nutting P, Smith JL, et al: Managing depression as a chronic disease: a randomised trial of ongoing treatment in primary care. British Medical Journal 325:934, 2002Crossref, Medline, Google Scholar
13. Wells KB: Caring for Depression. Cambridge, Mass, Harvard University Press, 1996Google Scholar
14. Murray CJL, Lopez AD (eds): The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability From Diseases, Injuries, and Risk Factors in 1990 and projected to 2020. Cambridge, Mass, Harvard University Press, 1996Google Scholar
15. Young AS, Klap R, Sherbourne CD, et al: The quality of care for depressive and anxiety disorders in the United States. Archives of General Psychiatry 58:55–61, 2001Crossref, Medline, Google Scholar
16. Wang PS, Berglund P, Kessler RC: Recent care of common mental disorders in the United States: prevalence and conformance with evidence-based recommendations. Journal of General Internal Medicine 15:284–292, 2000Crossref, Medline, Google Scholar
17. Mental Health: Culture, Race, and Ethnicity: A Supplement to Mental Health: A Report of the Surgeon General. Rockville, Md, Substance Abuse and Mental Health Services Administration, 2001Google Scholar
18. Mitchell K, Uehlinger KC, Owen J: The synergistic relationship between ethics and quality improvement: thriving in managed care. Journal of Nursing Care Quality 11:9–21, 1996Crossref, Medline, Google Scholar
19. Wolf S: Quality assessment of ethics in health care: the accountability revolution. American Journal of Law and Medicine 20:105–128, 1994Medline, Google Scholar
20. Piette M, Ellis JL, Denis PS, et al: Integrating ethics and quality improvement: practical implementation in transitional/extended care setting. Journal of Nursing Care Quality 17:35–42, 2002Crossref, Medline, Google Scholar
21. Field MJ, Lohr KN: Guidelines for Clinical Practice: From Development to Use. Washington, DC, Institute of Medicine, Committee on Clinical Practice, 1992Google Scholar
22. Pauly MV: Practice guidelines: can they save money? Should they? Journal of Law and Medical Ethics 23:65–74, 1995Google Scholar
23. Halpern J: Can the development of practice guidelines safeguard patient values? Journal of Law and Medical Ethics 23:75–81, 1995Google Scholar
24. Redman BK: Clinical practice guidelines as tools of public policy: conflicts of purpose, issues of autonomy, and justice. Journal of Clinical Ethics 5:303–309, 1994Medline, Google Scholar
25. Redman BK: Ethical issues in the development and use of guidelines for clinical practice. Journal of Clinical Ethics 7:251–256, 1996Medline, Google Scholar
26. Lohr KN: Guidelines for clinical practice: what they are and why they count. Journal of Law and Medical Ethics 23:49–56, 1995Crossref, Medline, Google Scholar
27. Povar GJ: What does "quality" mean? Critical ethical issues for quality assurance, in Striving for Quality in Health Care: An Inquiry Into Policy and Practice. Edited by Palmer RH, Donabedian A, Povar GJ. Ann Arbor, Mich, Health Administration Press, 1991Google Scholar
28. Smedley BD, Stith AY, Nelson AR, et al: Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC, National Academy Press, 2003Google Scholar
29. Capp S, Savage S, Clarke V: Exploring distributive justice in health care. Australian Health Review 24:40–44, 2001Crossref, Medline, Google Scholar
30. Sabin JE: General hospital psychiatry and the ethics of managed care. General Hospital Psychiatry 17:293–298, 1995Crossref, Medline, Google Scholar
31. Wells KB: The design of Partners in Care: evaluating the cost-effectiveness of improving care for depression in primary care. Social Psychiatry and Psychiatric Epidemiology 34:20–29, 1999Crossref, Medline, Google Scholar
32. Rubenstein LV, Jackson-Triche M, Unutzer J, et al: Evidence-based care for depression in managed primary care practices. Health Affairs 18(5):89–105, 1999Google Scholar
33. Wells KB, Sherbourne CD, Schoenbaum M, et al: Impact of disseminating quality improvement programs for depression in managed primary care: a randomized controlled trial. JAMA 283:212–220, 2000Crossref, Medline, Google Scholar
34. Halpern J: Reluctant patients: autonomy and delegating medical decisions. Journal of Clinical Ethics 13:78–84, 2002Medline, Google Scholar
35. Schneider C: The Practice of Autonomy: Patients, Doctors, and Medical Decisions. New York, Oxford University Press, 1998Google Scholar
36. Meredith LS, Jackson-Triche M, Duan N, et al: Quality improvement for depression enhances long-term treatment knowledge for primary care clinicians. Journal of General Internal Medicine 15:868–877, 2000Crossref, Medline, Google Scholar
37. Dwight-Johnson M, Unutzer J, Sherbourne C, et al: Can quality improvement programs for depression in primary care address patient preferences for treatment? Medical Care 39:934–944, 2001Google Scholar
38. Rawls J: A Theory of Justice. Cambridge, Mass, Belknap Press, 1971Google Scholar
39. Daniels N: Just Health Care. Cambridge, NY, Cambridge University Press, 1985Google Scholar
40. Miranda J, Azocar F, Organista KC, et al: Recruiting and retaining low-income Latinos in psychotherapy research. Journal of Consulting and Clinical Psychology 64:868–874, 1996Crossref, Medline, Google Scholar
41. Muñoz RF, Miranda J: Group Therapy for Cognitive Behavioral Treatment of Depression. Santa Monica, Calif, San Francisco General Hospital Depression Clinic, 1986Google Scholar
42. Muñoz RF, Aguilar-Gaxiola S, Guzmán J: Manual of Group Therapy for Cognitive-Behavioral Treatment of Depression [in Spanish]. Santa Monica, Calif, San Francisco General Hospital, 1986Google Scholar
43. Miranda J, Muñoz R: Intervention for minor depression in primary care patients. Psychosomatic Medicine 56:136–142, 1994Crossref, Medline, Google Scholar
44. Jacobson N, Dobson K, Turax P, et al: A component analysis of cognitive-behavioral treatment for depression. Journal of Consulting and Clinical Psychology 61:295–304, 1996Crossref, Google Scholar
45. Miranda J, Duan N, Sherbourne C, et al: Improving care for minorities: can quality improvement interventions improve care and outcomes for depressed minorities? Results of a randomized, controlled trial. Health Services Research 38:613–630, 2003Crossref, Medline, Google Scholar
46. Beauchamp TL, Childress JF: Principles of Biomedical Ethics. New York, Oxford University Press, 2001Google Scholar
47. Schoenbaum M, Unutzer J, Sherbourne C, et al: Cost-effectiveness of practice-initiated quality improvement for depression: results of a randomized controlled trial. JAMA 286:1325–1330, 2001Crossref, Medline, Google Scholar
48. Sherbourne CD, Wells KB, Duan N, et al: Long-term effectiveness of disseminating quality improvement for depression in primary care. Archives of General Psychiatry 58:696–703, 2001Crossref, Medline, Google Scholar
49. Unutzer J, Rubenstein L, Katon WJ, et al: Two-year effects of quality improvement programs on medication management for depression. Archives of General Psychiatry 58:935–942, 2001Crossref, Medline, Google Scholar
50. Jaycox LH, Miranda J, Meredith LS, et al: Impact of a primary care quality improvement intervention on use of psychotherapy for depression. Mental Health Services Research 5:109–120, 2003Crossref, Medline, Google Scholar
51. Schoenbaum M, Unutzer J, McCaffrey D, et al: The effects of primary care depression treatment on patients' clinical status and employment. Health Services Research 37:1145–1158, 2002Crossref, Medline, Google Scholar
52. Unutzer J, Katon W, Callahan CM, et al: Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA 288:2836–2845, 2002Crossref, Medline, Google Scholar
53. Gold MR: Cost-Effectiveness in Health and Medicine. New York, Oxford University Press, 1996Google Scholar



