Economic Grand Rounds: Systemwide Costs Associated With Second-Generation Antipsychotics in the Treatment of Schizophrenia
With the introduction of clozapine in the late 1980s, a new generation of antipsychotic medications became available for the treatment of schizophrenia. Although many studies of medication have compared average costs per patient in clinical trials (1) and in selected groups of patients (2), no study has examined the costs at the level of the service system, that is, relative to total mental health costs. In this study we examined a national sample of patients who were treated for schizophrenia in the Department of Veterans Affairs (VA) to determine the costs of first- and second-generation antipsychotic medications as a proportion of all mental health costs.
Methods
First, VA patients were identified who either received a diagnosis of schizophrenia on at least two outpatient visits between October 1, 2000, and September 30, 2001 (fiscal year 2001) or were discharged from an inpatient unit with a primary or secondary diagnosis of schizophrenia, schizophreniform disorder, or schizoaffective disorder (DSM-IV codes 295.00 to 295.99) (3). Second, all the mental health services delivered to these patients were identified by examining administrative databases, and costs were assigned by multiplying units of service by national average cost per unit (4). Third, all prescriptions for oral antipsychotic medications that were written within the VA for this group of patients during fiscal year 2001 were identified, and the total costs of these prescriptions for the VA were calculated. Because drug costs are substantially discounted in the VA, wholesale costs of these prescriptions were also calculated by using a ratio of VA to non-VA wholesale costs (5). Finally, the costs associated with various prescribing rates of first- and second-generation antipsychotics are presented.
Results
In fiscal year 2001, a total of 80,093 patients met the operationalized criteria for inclusion in the study. Figure 1 shows that more than $760 million was spent in providing mental health care to these patients in fiscal year 2001. Total costs of antipsychotic medications, based on the VA's discounted rate, were calculated to be nearly $94 million and represented 12.4 percent of all mental health costs, with $90 million (11.8 percent of all mental health costs) spent on second-generation antipsychotics.
If all the patients who received first-generation antipsychotics instead received second-generation antipsychotics, the cost of antipsychotics would rise to $134 million—an increase of $40 million—and the percentage of direct care dollars accounted for by antipsychotics would increase to 16.8 percent. However, if all the patients who received second-generation antipsychotics instead received first-generation antipsychotics, the cost of antipsychotics would fall to $11 million, or 1.6 percent of direct care dollars. The difference between these two scenarios is $124 million.
At wholesale prices, current prescriptions for antipsychotics would cost $175 million per year (21.3 percent of all mental health costs). If all the patients who received first-generation antipsychotics instead received second-generation antipsychotics at wholesale prices, the cost of antipsychotics would increase to $244 million dollars (26.8 percent of all mental health costs).
Discussion and conclusions
Within the VA, the cost of second-generation antipsychotics accounts for approximately 12 percent of $760 million in the direct medical care dollars that are devoted to the treatment of schizophrenia. The money spent on second-generation antipsychotics, first introduced approximately 15 years ago, represents a dramatic growth in medication expense. Although attempts have been made to manage expenditures for antipsychotics, they have not resulted in profound savings (6). Although the cost of antipsychotics has risen since the introduction of second-generation antipsychotics, overall expenditure on mental health within the VA has, in inflation-adjusted dollars, decreased by 25 percent since 1996 (7). Thus, with antipsychotic expenditures taking a large slice of a decreasing pie, spending in other areas, such as staffing, must almost inevitably suffer. Although spending 12 percent of mental health care dollars on antipsychotics was not an explicit goal of the VA administration, it is unclear how one would determine a priori what the optimal percentage of expenditure on medications would be—although a comparison of the benefits of increased spending for second-generation antipsychotics with the risks of decreased staffing or other expenditures would certainly be a crucial part of that determination.
These data also demonstrate the magnitude of the savings the VA realizes through its discounted drug prices. Federal law, through the establishment of the federal supply schedule, ensures that medications are made available to the VA at deeply discounted prices (8). Similar proposals at the state level have been highly contested (9) and have received much publicity recently, because some state-supported prescription plans, especially those supporting persons with serious mental illness, find themselves in serious financial difficulty (10).
Acknowledgment
This work was supported by the Mental Illness Research, Education, and Clinical Center of the VA New England Healthcare System.
Dr. Sernyak is associated with the psychiatry service and Dr. Rosenheck is with the Northeast Program Evaluation Center in the Department of Veterans Affairs Connecticut Healthcare System, 950 Campbell Avenue, West Haven, Connecticut 06516 (e-mail, [email protected]). Both authors are also affiliated with the department of psychiatry at Yale University School of Medicine in New Haven, Connecticut. Steven S. Sharfstein, M.D., and Haiden A. Huskamp, Ph.D., are editors of this column.
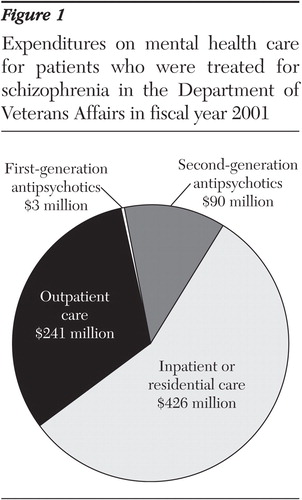
Figure 1. Expenditures on mental health care for patients who were treated for schizophrenia in the Department of Veterans Affairs in fiscal year 2001
1. Rosenheck R, Cramer J, Xu W, et al: A comparison of clozapine and haloperidol in hospitalized patients with refractory schizophrenia: Department of Veterans Affairs Cooperative Study Group on Clozapine in Refractory Schizophrenia. New England Journal of Medicine 337:809–815, 1997Crossref, Medline, Google Scholar
2. Lewis M, McCrone P, Frangou S: Service use and costs of treating schizophrenia with atypical antipsychotics. Journal of Clinical Psychiatry 62:749–756, 2001Crossref, Medline, Google Scholar
3. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
4. Rosenheck R, Cramer J, Allan E, et al: Cost-effectiveness of clozapine in patients with high and low levels of hospital use: Department of Veterans Affairs Cooperative Study Group on Clozapine in Refractory Schizophrenia. Archives of General Psychiatry 56:565–572, 1999Crossref, Medline, Google Scholar
5. Rosenheck R, Doyle J, Leslie D, et al: Changing environments and alternative perspectives in evaluating cost effectiveness of new antipsychotic drugs. Schizophrenia Bulletin 29:81–93, 2003Crossref, Medline, Google Scholar
6. Rosenheck R, Leslie D: Administrative prescription review procedures and use of atypical antipsychotic medications in the Department of Veterans Affairs. Mental Health Services Research 5:149–153, 2003Crossref, Medline, Google Scholar
7. Rosenheck R, Greenberg G: Department of Veterans Affairs National Mental Health Program Performance Monitoring System: Fiscal Year 2001 Report. West Haven, Conn, Northeast Program Evaluation Center, 2002Google Scholar
8. Drug Prices: Effects of Opening Federal Supply Schedule for Pharmaceuticals are Uncertain. Washington, DC, General Accounting Office, 1997Google Scholar
9. Sager A, Socolar D: Cutting Prescription Spending by Paying Federal Supply Schedule Prices. Boston, Health Reform Program, Boston University School of Public Health, 2000Google Scholar
10. Egan T: A prescription plan lauded as a model is a budget casualty. New York Times, Mar 5, 2003, pp 1Google Scholar



