Prescribers' Nonadherence to Treatment Guidelines for Schizophrenia When Prescribing Neuroleptics
Abstract
Treatment guidelines are frequently not followed. The authors examined the neuroleptic prescribing practices of psychiatrists responsible for 47 patients with schizophrenia who were being treated at health centers of the Department of Veterans Affairs. For 22 of these patients, a medication change was indicated by guidelines previously endorsed by the prescriber; for 21 of these 22 patients, prescribers indicated that a change in neuroleptic would not be attempted; for 15 patients (71 percent), the reason given was the patient's refusal to change medication or the patient's noncompliance with medication treatment. The results suggest that patients' agreement with treatment guidelines should be taken into account in the evaluation of prescribers' use of such guidelines.
Neuroleptic medications are firmly established as the primary treatment for the symptoms of schizophrenia. However, the atypical agents, such as clozapine, olanzapine, risperidone, and quetiapine, are expensive. One of the most common methods identified for maintaining—or even improving—the quality of care in the face of cost constraints has been the use of treatment guidelines.
Several guidelines or recommendations for the pharmacologic treatment of schizophrenia have been published in recent years (1,2,3,4). However, there is substantial evidence that treatment often does not adhere to these recommendations (5,6). The reasons for this discordance are unclear. Are clinicians unaware of these guidelines, or do they disagree with them? Are patients resisting indicated medication changes?
We chose to focus on a specific issue—the decision to switch neuroleptic medications for patients with schizophrenia. We chose this issue for two reasons. First, previous studies (5,6) indicated that, within the Department of Veterans Affairs (VA), many prescribers were not complying with the guidelines for prescribing neuroleptics. Second, a switch in neuroleptic medications can result in substantial improvement in symptoms.
This study was designed to determine prospectively whether psychiatrists changed their prescribing practices when they knew their behavior was being scrutinized, when they concurred with a set of treatment recommendations, and when, by the psychiatrists' own clinical assessment, these treatment guidelines indicated the need for a change in neuroleptic agent.
Methods
All the patients in the study had a diagnosis of schizophrenia or schizophreniform disorder and were receiving treatment at either the West Haven campus of the VA Connecticut Healthcare System (VACT) or the Connecticut Mental Health Center (CMHC), both of which are academic affiliates of Yale University. Institutional review board approval was obtained. All the patients provided written informed consent to having their treatment discussed by their clinician. Patients who were already receiving clozapine—that is, those at the end of the treatment algorithm—were excluded. The treatment described here occurred from April 1998 to July 2000.
All the prescribing psychiatrists who participated in the study were presented initially with a treatment algorithm that was thought to be both simple to follow and consistent with available standards. The first author—who is chief of psychiatry at VACT but holds no position of authority at CMHC—presented the algorithm to the treatment teams at each institution. The purpose and procedures of the prospective study were explained at that time. Views were solicited on whether the algorithm was not reasonable or not useful, but no dissent was voiced. Six months after each patient's enrollment in the study, the psychiatrists were interviewed by using a form (available from the first author on request) that evaluated four main elements of the neuroleptic treatment: the current treatment step, whether a change in neuroleptic medication was indicated on the basis of preestablished criteria, the medication change that was actually planned, and, if no change was planned, the reason for the lack of change.
The form was constructed to consist of a series of structured questions and responses, except for the section on the reasons for not changing medications. In that section, the prescribing psychiatrists were presented with a list of possible reasons for not changing medications and were instructed to endorse as many reasons as were clinically relevant or to add other reasons.
The treatment algorithm consisted of five steps: step 1, prescription of a conventional antipsychotic to the maximum tolerable dosage over a three-month period; step 2, prescription of a second conventional antipsychotic to the maximum tolerable dosage over a three-month period after the first agent failed; step 3, an atypical antipsychotic (risperidone, olanzapine, or quetiapine) to the maximum tolerable dosage over a three-month period; step 4, a second atypical antipsychotic to the maximum tolerable dosage over a three-month period after the first agent failed; and step 5, prescription of clozapine.
For the purposes of this study, a neuroleptic change was to be considered when the prescribing psychiatrist, using the Clinicians' Global Impression-Severity scale (7), rated the patient as being at least moderately ill (a score of 4 or more on a scale from 1, not at all ill, to 7, among the most extremely ill) and gave a change rating of minimally improved or less for the past six months (a score of 3 or more on a scale from 1, very much improved, to 7, very much worse).
The psychiatrists were then asked whether they agreed that a change in neuroleptic was indicated. If they did agree, they were asked whether they planned to attempt the change. If they said that an indicated change would not be attempted, they were asked to give all the relevant reasons.
Results
A total of 27 psychiatrists who were responsible for 47 patients were interviewed. All the psychiatrists indicated that they agreed with the proposed criteria for medication change and with the treatment algorithm. Of the 47 patients, 22 (47 percent) were rated by their psychiatrists as having symptoms that left them at least moderately ill and at best minimally improved.
At the time of assessment, for the 22 patients who met the operationalized criteria for change of neuroleptic medications, 11 (50 percent) were at step 1 of the algorithm, two (9 percent) were at step 2, seven (32 percent) were at step 3, none were at step 4, and one (5 percent) was at step 5—clozapine had been prescribed for this patient during the six-month study period. For 21 (95 percent) of these 22 patients, the psychiatrist indicated that although the patient met criteria for a change in medication, he or she did not plan to move the patient to the next step of the treatment algorithm. For each of the patients for whom the psychiatrist indicated that a change would not be made, the psychiatrist indicated all the reasons that the treatment would not progress according to the endorsed guidelines. These reasons are listed in Table 1.
The three leading reasons given for not progressing through the treatment algorithm were that the patient did not want to change (11 patients, or 52 percent), that the patient needed more time on the current medication (seven patients, or 33 percent), and that the patient was noncompliant with medications (six patients, or 29 percent). No psychiatrist raised the concern of violence as a reason for not proceeding with a medication change, and less than 10 percent were concerned about symptomatic decompensation.
Discussion and conclusions
After six months of treatment, 22 (47 percent) of the 47 patients with schizophrenia were judged by their prescribing psychiatrists as meeting operationalized criteria for a change in medication, suggesting that a change in neuroleptic medication was indicated. However, for only one (5 percent) of these 22 patients did the psychiatrist indicate that a change was being planned.
The psychiatrists in this study were aware of the proposed guidelines, had endorsed them, and rated the severity and duration of the patients' symptoms themselves. The psychiatrists' clinical impressions, combined with the relevant treatment guideline, indicated a change in neuroleptic. Yet overwhelmingly the psychiatrists did not institute such changes; for 15 (71 percent) of the 21 patients, either noncompliance or refusal of a recommended change was cited as the reason for not changing the medication. In fact, these reasons were two of the three most commonly cited reasons for not implementing the guideline recommendations.
The main limitation of this study was that it relied entirely on clinicians' self-report of their prescribing behavior. Thus we were unable to distinguish between two principal explanations for the fact that the patient's behavior was so frequently cited as the reason for noncompliance with the treatment recommendations. The psychiatrists may have falsely attributed resistance to change to the patient when asked to explain why they would not adhere to the treatment recommendations. Such an attribution would allow psychiatrists to appear to embrace good clinical practice as embodied by the treatment guidelines without actually changing their clinical behavior. However, it could also be that the psychiatrists were respectful of patients' wishes and deferred what they thought was the best course of treatment because of the patient's concerns. This possibility raises the question of what responsibility the clinician has to work with the patient to facilitate an indicated change.
Additional limitations included the small sample of psychiatrists interviewed and the fact that there were only two study sites. Also, the study did not examine the potential role of specific methods for addressing deviations from guidelines, such as computerized reminders (8).
The results of this study suggest that evaluating the real-world outcomes of treatment guidelines must take into account patients' agreement with the guidelines and the degree to which clinicians advocate for a course of treatment that they think is indicated.
Acknowledgment
This study was supported by the Mental Illness Research and Clinical Center of Veterans Integrated Service Network 1.
Dr. Sernyak is affiliated with the psychiatry service of the VA Connecticut Healthcare System and the department of psychiatry at Yale University School of Medicine in New Haven, Connecticut. Mr. Dausey is with the VA Northeast Program Evaluation Center and the Yale University School of Epidemiology and Public Health. Dr. Desai and Dr. Rosenheck are with the VA Northeast Program Evaluation Center and the department of psychiatry at the School of Medicine and the School of Epidemiology and Public Health at Yale University. Send correspondence to Dr. Sernyak, Psychiatry Service, 116A, VA Connecticut Healthcare System, West Haven Campus, 950 Campbell Avenue, West Haven, Connecticut 06516 (e-mail, [email protected]).
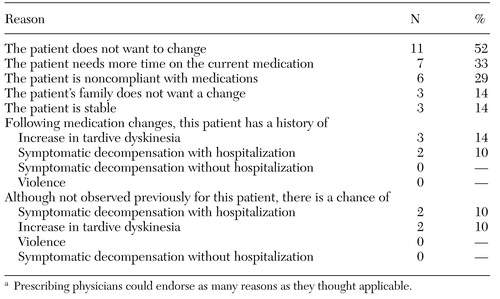 |
Table 1. but no dissent was voiced. Six Reasons given by prescribing physicians for not attempting a change in neuroleptic medication for 21 patients with schizophrenia or schizophreniform disordera
a Prescribing physicians could endorse as many reasons as they thought applicable.
1. Lehman AF, Steinwachs DM: At issue: translating research into practice: the Schizophrenia Patient Outcomes Research Team (PORT) treatment recommendations. Schizophrenia Bulletin 24:1-10, 1998Crossref, Medline, Google Scholar
2. American Psychiatric Association: Practice guideline for the treatment of patients with schizophrenia. American Journal of Psychiatry 154(Apr suppl):1-63, 1997Google Scholar
3. McEvoy JP, Weiden PJ, Smith TE, et al: Treatment of schizophrenia: the expert consensus guideline series. Journal of Clinical Psychiatry 57(suppl 12B):1-58, 1996Google Scholar
4. Chiles J, Miller A, Crismon M, et al: The Texas Medication Algorithm Project: development and implementation of the schizophrenia algorithm. Psychiatric Services 50:69-74, 1999Link, Google Scholar
5. Chen RS, Nadkarni PM, Levin FL, et al: Using a computer database to monitor compliance with pharmacotherapeutic guidelines for schizophrenia. Psychiatric Services 51:791-794, 2000Link, Google Scholar
6. Rosenheck RA, Desai R, Steinwachs D, et al: Benchmarking treatment of schizophrenia: a comparison of service delivery by the national government and by state and local providers. Journal of Nervous and Mental Disease 188:209-216, 2000Crossref, Medline, Google Scholar
7. Guy W: Clinical Global Impression, in ECDEU Assessment Manual for Psychopharmacology: US Department of HEW Publication 76-338. Edited by Guy W. Rockville, Md, Alcohol, Drug Abuse, and Mental Health Administration, 1976Google Scholar
8. Dexter P, Perkins S, Overhage M, et al: A computerized reminder system to increase the use of preventive care for hospitalized patients. New England Journal of Medicine 345:965-970, 2001Crossref, Medline, Google Scholar



