Recognition of Depression Among Elderly Recipients of Home Care Services
Abstract
OBJECTIVE: Depression among older home care patients is prevalent but undertreated. The purpose of this study was to investigate the ability of home health nurses to correctly identify depression among older patients and to describe nurse and patient characteristics associated with more accurate assessment of depression. METHODS: Forty-two nurses were surveyed about the presence of depressive symptoms among patients who had been evaluated independently for depressive disorders by research staff using the Structured Clinical Interview for Axis I DSM-IV Disorders. A sample of newly admitted home health care patients who were aged 65 years or older was randomly selected for this evaluation on a weekly basis from December 1997 to December 1999. RESULTS: Of 403 patients who were evaluated, 97 (24 percent) were found to have either major depression (64 patients) or minor depression (33 patients). The nurses correctly identified depression among 44 of the 97 patients who were depressed (sensitivity of 45.4) and 230 of the 306 patients who were not depressed (specificity of 75.2). The kappa coefficient measuring overall agreement between the nurses' assessment and the diagnosis of depression was .19. Nurses who had more geriatric nursing experience were more likely to correctly identify depression. CONCLUSIONS: Home health nurses have difficulty making accurate assessments of depression among older home care patients. Inaccuracy in assessment of depression by home health nurses is a significant barrier to treatment in this elderly homebound population.
Home health care has grown into a significant segment of the health care system for older persons. Home health nurses are pivotal to this system of care. The federal government pays for a majority of home health care services through Medicare and Medicaid programs (1). A requirement for federal reimbursement is a need for skilled nursing or rehabilitative therapy. Nurses provide care to 85 percent of home health care patients (2,3). According to the U.S. Bureau of Labor Statistics, 129,304 registered nurses and 40,849 licensed practical nurses worked at Medicare-certified home health agencies in 1998 (4). Despite evidence of the high rates of major depression among older persons with medical illness (5), home health nurses feel uncomfortable addressing psychiatric disorders (6). It is not known whether home health nurses can identify psychiatric illness in this growing population.
The decentralized structure of home health care further underscores the importance of the nurse's role in identifying depression among older patients. Physicians refer patients who need skilled nursing care to a home care agency that assigns a nurse to the case. The nurse travels to the patient's home to assess the patient's needs. These visits ordinarily follow hospitalization, the worsening of a chronic medical problem, or an accident. As part of the standard intake evaluation, nurses are required to note the presence of symptoms of depression. Because home health care delivery depends on the home health nurse's informing the treating physician of the status of the homebound patient, the inability of a home health nurse to recognize depression poses a significant potential barrier to treatment.
Recent data from a representative sample of geriatric home health care patients indicate that depression is highly prevalent in this population but is usually unrecognized and rarely treated (7). Failure to recognize and treat depression increases the risk of a prolonged course of depressive illness as well as the risk of suicide and mortality from other causes (8,9). The purposes of this study were to investigate the ability of home health nurses to correctly identify depression among older patients and to describe nurse and patient characteristics associated with more accurate assessment of depression.
Methods
The data for the study were collected from Visiting Nurse Services in Westchester (VNSW). VNSW is a nonprofit agency that has been accredited by the Community Health Accreditation Program, Inc., and serves a large county north of New York City. At the time of the study, VNSW was staffed by 43 registered nurses and ten social workers (all fee-for-service) as well as physical, speech, and occupational therapists and home health aides. Psychiatric nursing was provided by a cooperating agency. This study underwent a full review by and received approval from the institutional review board of Weill Medical College of Cornell University.
The VNSW nurses were surveyed about the presence of depressive symptoms among their patients who had been evaluated independently for depressive disorders by research staff using the Structured Clinical Interview for Axis I DSM-IV Disorders (SCID) (10). Newly admitted home health care patients aged 65 years or older were randomly selected for this evaluation on a weekly basis over a two-year period—December 23, 1997, to December 19, 1999. After ineligible patients had been excluded from the sampling frame (those who spoke neither English nor Spanish and those who were unable to give informed consent), a 40 percent sample of 889 patients was selected.
Of the 889 patients who were invited to participate in the study, 539 (61 percent) provided signed consent. Aggregate data provided by the agency indicated that, on average, the patients who agreed to participate were significantly younger than those who refused (78.3 years compared with 80.2 years, p<.001) but did not differ significantly by gender, nurse-reported mental status (for example, disoriented, forgetful, or depressed), prognosis, or referring diagnosis.
Measures
The data reported come from interviews with patients, interviews with informants (for example, a person living with the patient), VNSW medical records, a nursing staff survey, and a patient-specific nursing survey.
Best-estimate procedures were used in making SCID diagnoses of depression. The assessments were conducted by research assistants who had been trained to reliability. On average, the assessments occurred three weeks (21.2±6.8 days) after the start of home health care services. Informants were interviewed when available. Information from the patient's SCID interview, the informant's SCID interview, the home care medical record, and medication schedules were evaluated in a best-estimate conference that included a geriatric psychiatrist, a psychologist, a medical internist, and the study's principal investigator to determine diagnostic status. For the purpose of the analyses presented here, depression was defined as a DSM-IV diagnosis of major or minor depression regardless of medical etiology (11,12).
Patients' sociodemographic variables included self-reported age, race, income, and living arrangements. Health-related variables included cognitive status as measured by the Mini Mental State Examination (13), ICD-9 diagnoses responsible for home care admission as reported on the medical record, medical severity based on the Charlson Comorbidity Index (CCI) (14) as coded by the study's medical internist; disability as measured by counts of limitations in activities of daily living (15) and instrumental activities of daily living (16), and intensity of pain, which was assessed by the single three-level item from the Short-Form-36 Health Survey (SF-36) (17). Information on use of antidepressants was obtained from VNSW medical records and augmented by review of patients' medications in the home interview.
Each nurse completed a nursing staff survey that collected demographic information, including data on gender, formal education, licensure, home health care experience, and geriatric nursing experience. Quartile scores were used to categorize nurses' geriatric nursing experience as novice (zero to three years), intermediate (four to ten years), experienced (11 to 17 years), or expert (18 or more years).
A patient-specific nursing survey was developed for this study, pilot-tested by eight nurses, and modified for clarity. The primary purpose of the patient-specific nursing survey was to obtain the nurses' opinions on the depressive status of their patients. In routine practice, home health nurses are not expected to diagnose depression but instead to assess for the individual signs and symptoms of the depressive syndrome. Nurses were asked, "In your opinion, is this patient depressed?" If the response was yes, the nurse was asked, "How significant is the depression in this patient?" To answer these questions, the nurses were presented with a 3-point Likert scale on which to rate depression as severe, moderate, and mild.
To determine whether a nurse was able to identify depressive symptoms consistent with a clinically significant depressive syndrome, the nurse's rating of depression as either severe or moderate was compared with the DSM-IV diagnosis of major or minor depression. The number of nursing visits that each patient received and the number of days since the nurse's last visit were also obtained. On average, the survey was conducted 15.1±12.4 days after the initial patient interview. Nurses who were inaccessible for a face-to-face interview were interviewed by telephone. Both the individual who interviewed the nurse (the first author) and the nurse were blinded to the results of the initial patient interview.
Data analysis
The agreement between nurses' ratings of depression and the depression diagnosis identified by best-estimate procedures (the presumed standard) was estimated by using the kappa statistic, a measure of agreement corrected for chance (18). The sensitivity and specificity of the nurses' reports of depression were calculated by using the best-estimate diagnosis of depression.
Nurse and patient characteristics associated with the level of agreement between nurses' ratings and the best-estimate measure of depression were examined in two sets of analyses. The first examined whether nurses correctly identified depression among patients who had a DSM-IV diagnosis of depression. The second examined whether nurses incorrectly identified depression among the patients who did not have a diagnosis of depression.
Both sets of analyses compared patients whom the nurses identified as being depressed with the patients who were not identified as depressed by using chi square tests for categorical measures and t tests for continuous measures of nurse and patient characteristics. In each set of analyses, logistic regression models were used to estimate whether the relevant patient and nurse characteristics were independently associated with agreement between nurses' ratings and the best-estimate diagnosis. Initially, separate logistic regression models were estimated for each nurse and patient characteristic. If the univariate model resulted in a p value below .25, the variable was included in a multivariate model (19). Likelihood ratio tests were conducted for each measure, and variables with significance levels above .15 were eliminated from the multivariate model by using a stepwise procedure.
Because it was possible for each nurse to rate more than one patient, the usual assumption of independent observations did not hold for these analyses. Therefore, all significance testing was conducted with Taylor series linearization procedures as implemented in the SUDAAN software (20) to account for the nonindependence of ratings.
Results
Nurse characteristics
Forty-two nurses completed 403 of a potential 539 patient-specific nursing surveys, for a response rate of 75 percent. These nurses provided skilled nursing care and case management for each of the 403 home health care patients. One nurse declined the invitation to participate in any surveys. Other common reasons for patient-specific interviews not being conducted were extended leave or inability to contact the nurse (56 interviews) and the fact that the nurse did not remember the patient (23 interviews). The nurses were primarily women (93 percent), and all had their registered nurse licensure. The mean number of years of geriatric nursing experience was 12.6±9.7, and the mean number of years of home health nursing experience was 7±6.9. Twenty-four nurses (58 percent) had obtained a baccalaureate degree, and nine nurses (21 percent) had completed a master's degree.
Patient characteristics
Of the 403 patients, a majority were female (268 patients, or 67 percent) and white (342 patients, or 85 percent). The patients ranged in age from 65 to 98 years, and their mean age was 78.7±7.32 years. A total of 161 patients (40 percent) were married, and 160 (40 percent) lived alone. A total of 376 (95 percent) reported at least one disability in instrumental activities of daily living, and 214 (54 percent) reported at least one disability in activities of daily living. The patients' mean score on the CCI was 2.8±2.05, indicating a substantial medical burden. (Possible scores on the CCI range from 0 to 11, with higher scores indicating more severe comorbidity.) Furthermore, 108 patients (27 percent) reported experiencing "a great deal" of pain since the initiation of home care services. A majority of the patients had traditional Medicare insurance. Twenty-eight patients (7 percent) had a principal ICD-9 diagnosis of congestive heart failure (code 428.0), 21 patients (5 percent) had chronic airway obstruction (code 496), 20 patients (5 percent) had an open wound or wounds (code 879.8), and 15 patients (4 percent) had heart disease, unspecified (code 429.9). Of the 403 patients, 97 (24 percent) met DSM-IV criteria for either major depression (64 patients) or minor depression (33 patients).
Nurses' assessment of depression
Under the assumption that the best-estimate measure provided a true evaluation of a patient's depressive status, 274 patients (68 percent) were accurately classified by the nurses. The nurses correctly identified 44 of the 97 patients with depression (a sensitivity of 45.4) and 230 of the 306 patients who did not have depression (a specificity=75.2). Of the 44 patients who were correctly identified as having depression, 28 had major depression (a sensitivity of 43.7) and 16 had minor depression (a sensitivity of 48.5). Chance-corrected agreement between the nurses' assessment and the best-estimate measure of depression was poor (kappa=.19).
Predictors of accuracy
Nurse and patient characteristics were examined to identify the factors associated with more accurate assessment of depressed patients and those who were not depressed. The nurses' accuracy in identifying depression among depressed patients (sensitivity) is summarized in Table 1 by nurse and patient characteristics. The patient characteristics that were significantly associated with correct identification of depression among the 97 patients who were depressed included living situation and disability in activities of daily living. Nurses were more likely to recognize depression among depressed patients who were not living alone and who had two or more disabilities in activities of daily living. Geriatric nursing experience was also positively associated with accuracy: accurate assessment of depression was significantly more likely among nurses who were classified as intermediate, experienced, or expert. Neither the number of patient visits nor the number of days since the last nursing visit were significantly associated with accurate assessment.
The variables retained in the multivariate model of sensitivity were female gender (odds ratio [OR]=3.21, 95% confidence interval [CI]=1.28 to 8.07), not living alone (OR=3.12, 95% CI=1.18 to 8.32), having two or more disabilities in activities of daily living (OR=2.32, 95% CI=.96 to 5.56), and geriatric nursing experience (intermediate, OR= 2.63; experienced, OR=3.95; and expert, OR=5.37).
The nurses' accuracy in identifying patients who were not depressed (specificity) is summarized in Table 2 by nurse and patient characteristics. Three patient characteristics were significantly associated with incorrect identification of depression among the 306 patients who did not have depression: use of antidepressants, patient reports of a great deal of pain, and intact cognitive functioning. None of the nursing factors were associated with incorrect identification of depression. The variables retained in the multivariate model of specificity were living alone (OR=.60, 95% CI=.36 to 1.00), use of antidepressants (OR=.19, 95% CI=.08 to .45), and having a great deal of pain (OR=.44, 95% CI=.25 to .76).
Discussion and conclusions
Unless home health nurses are able to accurately and routinely assess patients for signs and symptoms of depression, depression will remain a significant health problem for home health patients. The results of this study indicate that home health nurses have difficulty distinguishing between older patients who have a DSM-IV diagnosis of a depressive disorder and those who do not. Consequently, depression is missed among many elderly patients.
The many factors that complicate screening for depression among elderly patients are well documented. In geriatric home care, the only nurse characteristic that was associated with more accurate assessment of depression was the extent of geriatric nursing experience. This finding suggests that education may help improve the accuracy of assessment. Of all the patient characteristics investigated, disability in activities of daily living and living with another person were associated with more accurate identification of depression. Nurses may correctly associate disabilities with depression and may use informants—for example, a person who is living with the patient—to help in the recognition of depression.
Three patient factors predicted the incorrect identification of depression by nurses among patients who were not depressed: living alone, using antidepressants, and reporting a great deal of pain. The nurses may view patients who live alone as being isolated and lonely and thus possibly depressed. A possible explanation for the finding about antidepressant use is that the nurses believed that if an antidepressant had been prescribed for a patient, the patient must have been experiencing depressive symptoms. Patients who were not depressed but who reported having a great deal of pain were incorrectly identified as being depressed. It may be that the nurses linked pain, a known risk factor for depression (21), to depression itself. These findings further suggest a need to clarify the etiology, clinical presentation, and course of depression in educational programs for nurses.
Routine screening for signs and symptoms of depression is an expected standard of home health nursing practice. Yet we found that nurses missed depression among more than half of the patients who met diagnostic criteria for depression. Home health nurses are burdened with extensive mandatory patient assessments, some of which—especially the Outcome and Assessment Information Set (OASIS)—already expect nurses to assess for symptoms associated with depression. Adding a standardized screening instrument is an attractive solution but may lead to increased workload and thus might not be feasible in this setting.
An alternative strategy may be to enhance nurses' abilities in using their current sets of assessments. Asking about the psychological and somatic symptoms of depression is compatible with routine care and, combined with additional training for nurses, is likely to improve their recognition of depressive disorders (22). The incorrect identification of patients who were not depressed as being depressed was also a problem (specificity of 75.2), although it was no worse than has been observed with the use of many structured checklists. For example, the specificity of the short from of the Geriatric Depression Scale was 74 percent in a geriatric affective disorders outpatient clinic (23). By educating nurses on how to recognize depression, the problem of misidentification may also diminish.
Given that treatment of depression has been shown to improve the overall health of elderly patients (24), recognition of signs and symptoms consistent with a depressive disorder should signal the need for further evaluation by the treating physician, psychiatric nurse, social worker, or other mental health provider. There is also a critical need for training in the area of when and how to make referrals to these other professionals. The home health agency in this study did not have a mental health division at the time data were collected. Patients who required a psychiatric nurse were referred to a mental health division in another agency.
Partially in response to the findings of this study, VNSW has since established a mental health division and has incorporated recognition of symptoms of depression into the routine training of its nursing staff. Individual quality improvement programs are an important step; however, this step alone will not solve the problem. Improved screening for depression throughout the home care industry will require a change in the prospective payment system, which currently does not include symptoms of depression in reimbursement calculations.
Improving the recognition and treatment of depression in this elderly, homebound, sick population is complicated. Home health nurses are uniquely placed to assess psychological status and provide information on how the patient functions in his or her home environment. However, in most cases home health nurses do not have regular access to mental health expertise. Research is needed to develop intervention strategies that use a multidisciplinary approach to improve treatment of depressive disorders among older home health care patients.
Acknowledgment
This study was supported by grants RO1-MH-56482, T32-MH-19132, and KO2-MH-01634 from the National Institute of Mental Health.
Dr. Brown, Dr. McAvay, Dr. Raue, and Dr. Bruce are affiliated with the department of psychiatry at Weill Medical College of Cornell University, 21 Bloomingdale Road, White Plains, New York 10605 (e-mail, [email protected]). Ms. Moses is with Visiting Nurse Services in Westchester in White Plains. A version of this paper was presented at the annual meeting of the American Association for Geriatric Psychiatry held March 12-15, 2000, in Miami.
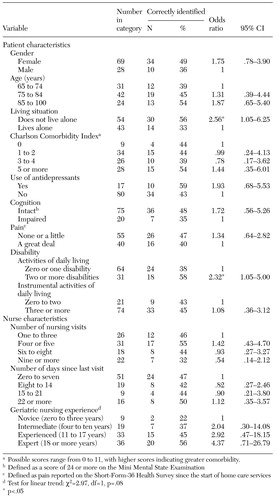 |
Table 1. Accuracy of home health care nurses in identifying depression in a sample of 97 elderly home care patients who had a DSM-IV diagnosis of major or minor depression
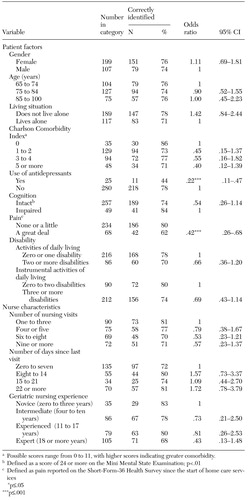 |
Table 2. Accuracy of home health care nurses in identifying patients who were not depressed in a sample of 306 elderly home care patients who did not have a DSMIV diagnosis of major or minor depression
1. National Health Expenditure Projections:1998-2008, Freestanding Home Health Agencies. Health Care Financing Administration, Office of the Actuary. Available at www.hcfa.govGoogle Scholar
2. Munson ML: Characteristics of Elderly Home Health Care Users: Data From the 1994 National Home and Hospice Care Survey. Advanced Data From Vital and Health Statistics, no. 309. Hyattsville, Md, National Center for Health Statistics, 1999Google Scholar
3. Kramarow E, Lentzner H, Rooks R, et al: Health and Aging Chartbook: Health, United States, 1999. Hyattsville, Md, National Center for Health Statistics, 1999Google Scholar
4. National Industry-Occupational Employment Matrix. Washington, DC, Bureau of Labor Statistics, 1998Google Scholar
5. Dew MA: Psychiatric disorder in the context of physical illness, in Adversity, Stress, and Psychopathology. Edited by Dohrenwend BP. New York, Oxford University Press, 1998Google Scholar
6. Carson V: Depression as a complicating factor for home care patients. Caring 20:30-33, 2001Medline, Google Scholar
7. Bruce ML, McAvay GJ, Raue PJ, et al: The epidemiology of major depression in elderly home health care patients. American Journal of Psychiatry 159:1367-1374, 2002Link, Google Scholar
8. Lebowitz BD, Pearson JL, Schneider LS, et al: Diagnosis and treatment of depression in late life: consensus statement update. JAMA 278:1186-1190, 1997Crossref, Medline, Google Scholar
9. Unutzer J, Katon W, Sullivan M, et al: Treating depressed older adults in primary care: narrowing the gap between efficacy and effectiveness. Milbank Quarterly 77:225-241, 1999Crossref, Medline, Google Scholar
10. Spitzer RL, Gibbon M, Williams JB (eds): Structured Clinical Interview for Axis I DSM-IV Disorders (SCID). Washington, DC, American Psychiatric Association, 1995Google Scholar
11. Koenig HG, George LK, Peterson BL, et al: Depression in medically ill hospitalized older adults: prevalence, characteristics, and course of symptoms according to six diagnostic schemes. American Journal of Psychiatry 154:1376-1383, 1997Link, Google Scholar
12. Mulsant BH, Ganguli M: Epidemiology and diagnosis of depression in late-life. Journal of Clinical Psychiatry 60(suppl 20):9-15, 1999Medline, Google Scholar
13. Folstein MS, Folstein SE, McHugh PR: Mini Mental State: a practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research 12:189-198, 1975Crossref, Medline, Google Scholar
14. Charlson ME, Pompei P, Ales KL, et al: A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Diseases 40:373-383, 1987Crossref, Medline, Google Scholar
15. Katz S, Downs TD, Cash HR: Progress in the development of an index of ADL. Gerontologist 10:10-20, 1970Crossref, Google Scholar
16. Lawton MP, Brody EM: Assessment of older people: self-maintaining instrumental activities of daily living. Gerontologist 9:179-186, 1969Crossref, Medline, Google Scholar
17. Ware JE, Sherbourne CD: The MOS 36-Item Short Form Health Survey (SF-36): I. conceptual framework and item selection. Medical Care 30:473-483, 1992Crossref, Medline, Google Scholar
18. Fleiss JL: Statistical Methods for Rates and Proportions, 2nd ed. New York, Wiley, 1981Google Scholar
19. Hosmer DW, Lemeshow S: Applied Logistic Regression. New York, Wiley, 1989Google Scholar
20. Shah BV, Barnwell BG, Bieler GS: SUDAAN User's Manual, Release 7.0. Research Triangle Park, NC, Research Triangle Institute, 1996Google Scholar
21. Parmelee PA, Katz IR, Lawton MP: The relation of pain to depression among institutionalized aged. Gerontology 46:15-21, 1991Crossref, Google Scholar
22. Brown E, Raue P, Nassisi P, et al: Increasing recognition and referral of the depressed elderly. Home Healthcare Nurse 19:558-564, 2001Crossref, Medline, Google Scholar
23. Herrmann N, Mittmann N, Silver I, et al: A validation study of the geriatric depression scale short form. International Journal of Geriatric Psychiatry 11:457-460, 1996Crossref, Google Scholar
24. Mental Health: A Report of the Surgeon General: Executive Summary. Rockville, Md, US Department of Health and Human Services, 1999Google Scholar



