Clinical and Forensic Outcomes From the Illinois Mental Health Juvenile Justice Initiative
Abstract
OBJECTIVE: To address the mental health needs of youths who are arrested and detained in Illinois, an initiative was designed and implemented that identified youths with psychotic or affective disorders, linked them to community services, and monitored their cases. This study assessed whether such linkage is possible and whether it improves clinical and forensic outcomes. METHODS: Under the initiative, court staff refer youths who may have a mental illness to a clinical liaison. If the youth is eligible for the program, the liaison works with the family to develop a community-based action plan. For the analysis presented here, the Child and Adolescent Needs and Strengths-Mental Health Scale (CANS-MH) and the Child and Adolescent Functional Assessment Scale (CAFAS) were used to assess outcomes among 314 youths who had completed the program at the time of the study. School and forensic outcomes were also monitored. RESULTS: Seventy-five percent of the youths were successfully linked to at least one mental health or community service. A comparison of average CANS-MH dimension scores at enrollment and program completion indicated that youths' emotional problems decreased considerably within three months of referral. CAFAS scores six months after enrollment improved across nearly all dimensions. Home, community, and school functioning were significantly improved from baseline. Only 42 percent of the youths were rearrested, compared with a statewide rate of 72 percent of detained youths. CONCLUSIONS: By linking youths with significant mental health needs to existing community-based services, it appears possible both to ameliorate psychopathology and to reduce delinquency.
A notable proportion of youths who are involved in the juvenile justice system have significant mental health needs (1,2). A project funded by the National Institute of Mental Health found that 66 percent of such youths had a diagnosable psychiatric condition and that about 15 percent could be described as having a major mental illness, such as a major depressive episode or psychosis (3). After substance-related and conduct disorders, both of which involve delinquent behavior, forms of depressive disorders were the next most common psychiatric disorders. With an estimated 2.5 million youths arrested each year (4), the number of youths with psychiatric needs in the juvenile justice system is substantial.
Although the high level of mental health need among detained youths has been substantiated, less is known about effective strategies for addressing these needs (5). The best-known evidence-based practice for juvenile offenders is multisystemic treatment (6,7,8). However, this treatment is intensive and expensive and has focused on youths with disruptive behavioral disorders rather than those with serious mental illness. Other approaches include mental health courts (9) and wraparound approaches consistent with system-of-care philosophy (10,11,12).
On the basis of the U.S. Surgeon General's conference report (13), there is some reason for optimism that traditional mental health interventions of psychotherapy and medication management are likely to be effective with youths who have depression and psychosis. In some cases, juvenile justice is the first agency to become involved with the youth; in other cases, previous failures of community-based treatment, often reportedly due to youth and family noncompliance, are associated with delinquency (14,15,16).
These data suggest that if youths in detention were identified as having an affective or psychotic disorder, effective linkage with existing mental health treatment providers will prove clinically effective, possibly preventing further delinquency. This was the thinking behind the development of the Mental Health Juvenile Justice (MHJJ) initiative in Illinois.
In this article we present evaluation data from the MHJJ initiative to address the following four questions. First, can youths with affective or psychotic disorders who are in juvenile detention centers be identified and recruited for mental health treatment? Second, can these youths be effectively linked to community-based treatment? Third, does this linkage result in an improvement in these youths' mental health? Finally, do these youths become less likely to be rearrested or detained in the future?
Methods
Program background and design
The MHJJ initiative was started by the division of mental health of the Illinois Department of Human Services in seven counties in March 2000. Eligibility is determined by the presence of either a psychotic disorder or an affective disorder. Juveniles with disruptive behavior disorders are excluded unless these disorders are comorbid with psychotic or affective disorders. In 2001 MHJJ was expanded to all counties with detention centers and one county that recently closed its detention center, for a total of 16 detention centers located throughout the state.
The program design has court staff—for example, judges, attorneys, probation officers, and detention center staff—referring a youth who may have a mental illness to the MHJJ clinical liaison. A simple yes-or-no instrument developed by the evaluation team was provided to help court staff decide whether to make a referral. However, some court staff used existing strategies—for example, intake assessments and observations.
Once a youth is referred to MHJJ, the liaison contacts the youth's parents for permission to screen the youth and communicate with the court about MHJJ involvement. If permission is granted, the liaison meets with the youth and assesses him or her for the presence of an affective or psychotic disorder on the basis of DSM-IV criteria (17). If the youth is eligible, the liaison works with the family to develop a community-based action plan. The plan is wraparound in design, including individualized services that address the youth's needs and strengths. Once services are identified, the liaison arranges funding. If the services are not covered by private or public funding, the liaison has access to a flexible fund as a supplement. The liaison's involvement is intended to be for up to six months, although the services to which the youth is linked would be expected to continue after the liaison's involvement.
The liaison does not function as an agent of the court but does inform the court that there is a youth in detention with a major mental illness who has certain needs and that these needs can be met by specific services in the community. Should the court decide to release the youth to the community, the liaison works with the family to establish linkages with the community providers. The liaison is not to interfere in the court case regarding the youth's guilt, innocence, fitness, or sanity. Also, the liaison does not provide direct treatment.
Evaluation design
The evaluation design involved an outcomes management approach to support the operations of the program at each site. As noted, a brief screening measure was created to help court staff identify potential referrals to the program. The liaisons used the Childhood Severity of Psychiatric Illness (CSPI) to assess eligibility (18,19). The CSPI, although not a diagnostic tool, is designed to be consistent with psychiatric diagnoses and is familiar to many of the Illinois providers (20). All liaisons were trained to a reliability of above .80. Once a youth is determined to be eligible, the provider completes the Child and Adolescent Needs and Strengths-Mental Health Scale (CANS-MH) (21,22). The CANS-MH is a service-planning tool that allows for assessing outcomes. The CANS-MH is completed for youths at enrollment, at three months, and at six months. Finally, providers completed the Child and Adolescent Functional Assessment Scale (CAFAS) (23,24) at initiation and termination of services.
Providers also complete monthly reports on services provided, school attendance and suspensions, and new arrests and detentions for all open cases. An annual audit methodology (25) was used to monitor reliability of the CANS-MH. Audit reliability measures averaged around .80.
Results
Description of participants
Most of the 314 youths in this sample were male (214 youths, or 68 percent), and their age range was ten to 17 years. A majority were aged 14 to 16 years (251 youths, or 80 percent). More than half were white (179 youths, or 57 percent), slightly more than one-third were African American (108 youths, or 34 percent), and 16 (5 percent) were Hispanic. Most (261 youths, or 83 percent) were living at home with their biological parents at the time they were arrested. Youths who were in state custody were not eligible for the MHJJ initiative. Most of the youths in the sample were enrolled in school at the time of arrest (252 youths or 80 percent), but only 142 (45 percent) were classified as special-education students. A majority (238 youths, or 76 percent) had received mental health treatment before their contact with an MHJJ liaison, and 84 (27 percent) had previously received treatment for substance abuse.
Diagnoses were provided by the liaison on the basis of an interview with the youth. Affective disorders without psychosis were more common than psychotic disorders (236 youths, or 75 percent, compared with 78 youths, or 25 percent). Among the psychotic disorders, affective disorders with psychosis were the most common. Only six youths (2 percent) were determined to have some form of schizophrenia.
Crimes for which the detention resulted were varied. Forms of battery were the most common (82 youths, or 26 percent), followed by parole or probation violations (39 youths, or 12 percent).
Identification and referral
A total of 1,885 youths were referred for screening. Liaisons successfully contacted parents of those youths, of whom 1,553 (82 percent) consented to further screening of their children for eligibility. After screening with the CSPI, 837 youths were found eligible for the program. Thus approximately 54 percent of the 1,553 youths screened positive for either psychotic or affective symptoms of at least moderate intensity. Youths who were deemed ineligible for participation were primarily those with disruptive behavior problems only or mild symptoms of depression without associated functional impairment. Of the eligible youths, 668 (80 percent) were enrolled and participated in initial service planning. Of these, 314 had completed participation in the program at the time of the analyses reported here. Of the closed cases, 256 (82 percent) had at least one follow-up CANS-MH assessment.
Service linkage and use
The mean±SD time spent by the liaison per service episode was 19±19.7 hours. Sixty-three percent of this time was spent in direct contact with the youth or the youth's family. However, the variation across the 314 youths was dramatic—six youths (2 percent) received no services, and one received 155 hours of services. The median time spent per case was 13.5 hours. On average, liaisons provided about four home visits per case, although 40 youths (13 percent) received no home visits. Of the closed cases, 45 (14 percent) were served for less than one month, 47 (15 percent) for one to two months, 47 (15 percent) for three to four months, 115 (37 percent) for five or six months, and 37 (12 percent) for more than six months.
More than half (177 youths, or 56 percent) received individual counseling services. The number of sessions attended during participation in the program ranged from one to 62, with a median of six sessions. More than one-third (122 youths, 39 percent) met with a psychiatrist for medication management. A smaller proportion received group counseling (42 youths, or 13 percent). Over the service episode, 44 youths (14 percent) were psychiatrically hospitalized. Eight percent (25 youths) received individual substance abuse counseling services, and 18 (6 percent) received group substance abuse counseling. Overall, 235 youths (75 percent) were successfully linked to at least one mental health or community service.
Mental health outcomes
The emotional problems of youths enrolled in the MHJJ initiative decreased considerably within three months of their referral. A comparison of average CANS-MH dimension scores at enrollment and at program completion is shown in Table 1. When a youth received more than two CANS assessments, the first and last assessment were used for these analyses.
Table 2 shows the changes in scores for individual items on problems, risk behaviors, and functioning from the CANS-MH at enrollment and at program completion. Ratings of 2 and 3 on individual items of the CANS-MH can be considered actionable levels of need—an intensity that requires some intervention. In addition to showing improvements on the two eligibility items—psychosis and depression or anxiety—youths also improved on other mental health needs. Youths demonstrated less danger to others, sexually abusive behavior, and crime or delinquency. No declines were noted for the other risk behaviors. Improvements in functioning were observed in family, school, and sexual development.
CAFAS scores six months after enrollment in MHJJ demonstrate improvements across nearly all dimensions. The total CAFAS score declined over the course of the MHJJ initiative. Children's functioning in the home, in the community, and in school was significantly improved from baseline scores. Only the CAFAS substance use subscale did not show significant improvement over time.
The reduction in problems among youths with psychosis was nearly twice the magnitude of that for youths with affective disorders (t=4.42, df=254, p=.006). Youths with affective disorders experienced a significantly greater improvement in strengths at program termination (t=2.27, df=254, p=.025).
Forensic outcomes
Of the 314 MHJJ youths who were included in the evaluation study, 132 (42 percent) were rearrested. This figure is considerably lower than the rearrest rate of 72 percent of all youths arrested and detained that has been reported for Illinois (26). For youths who were provided with direct services from the liaison for more than one month, the rearrest rate was only 29 percent.
Youths who were rearrested were compared with those who were not on each of the CANS-MH items at enrollment. All the items that were statistically significant in this univariate comparison were entered into a logistic regression model predicting rearrest. The overall model was statistically significant (χ2=38.19, df=10, p<.001), accurately classifying 68 percent of youths. The significance of individual CANS-MH items is shown in Table 3. Four items stand out as contributing uniquely to the prediction model—runaway risk, sexually abusive behavior, religious or spiritual strengths, and talents and interests. Runaway risk increased the likelihood of rearrest. The presence of sexually abusive behavior was associated with a decreased risk. The presence of spiritual or religious strengths and of talents and interests were associated with a decreased risk of rearrest. No CAFAS scale scores predicted rearrest.
Youths who demonstrated greater improvements in symptoms and risk behavior over the first three months of the intervention were less likely to be rearrested. Specifically, among youths who were not rearrested, the mean change scores on CANS-MH items were more than twice those of youths who were rearrested (t=3.02, df=254, p=.003). The improvement in risk behaviors as measured by mean CANS-MH scores among these youths was nearly three times that of youths who were rearrested (t=3.26, df=254, p=.001).
School outcomes
Sixty-three youths (20 percent) were suspended from school during the service episode. Predictors of suspension were a lower level of substance abuse (t=-2.74, d=312, p=.006), greater consistency of symptoms over situations (t=2.19, df=312, p=.03), lower crime or delinquency (t=-2.52, df= 312, p=.01), and fewer vocational strengths (t=2.21, df=312, p=.02).
Discussion
The results of this study support the hypotheses that by identifying, referring, and monitoring arrested and detained youths who have either affective or psychotic disorders, positive mental health and forensic outcomes can be achieved. It is clear that a sufficient number of youths with these conditions could be identified in the 16 detention centers throughout Illinois. Furthermore, it appears that these youths could be successfully linked to mental health and other services in their community. Linking these youths was associated with improved mental health, reduced risk behaviors, improved functioning, and an increase in identified strengths. Finally, these youths appeared to be less likely to return to the juvenile justice system through arrest and detention. The greater the success of the mental health treatment, the less likely the youth was to be rearrested or placed in detention. The overall rate of success is comparable to that reported by multisystemic treatment (6,7,8). However, this comparison should be made cautiously, given that MHJJ and multisystemic treatment are designed to serve different clinical populations.
The fact that successful reduction of problems and risk behaviors during the first three months of the intervention predicted whether a youth was rearrested may shed some light on the mechanism of the effectiveness of this intervention. If resolving mental health needs reduces delinquent behavior, then a causal link between mental health and delinquency is supported. The success of this intervention may be due to its ability to link identified youths with effective community treatment. Thus secondary prevention of delinquency for youths with these psychiatric conditions would be effective psychiatric treatment. Because these youths have serious mental health needs and only 39 percent were successfully linked with a psychiatrist, one wonders whether the results would be even better if this linkage could be improved.
The clinical implications of this research are fairly clear. Ensuring that detained youths with mental health needs are identified and linked to community-based services should be a priority. It appears that for these youths, linkage to existing community-based mental health services may be sufficient. However, the characteristics of youths who were rearrested suggest opportunities for service development. Two findings stand out. First, the importance of parental characteristics is clear. Second, the role of strengths in preventing rearrest is provocative. The role of spirituality or religion is intriguing and offers some support for faith-based initiatives. The fact that talents and interests and vocational strengths at baseline were associated with success at preventing future arrests suggests that expanding services to build these strengths could be important.
Contrary to the folklore about the lack of involvement of parents of youths in the juvenile justice system, most of the parents in this study consented to their child's involvement and participated in the service planning process. However, caregivers' needs and strengths did not improve over the course of the intervention, probably because the intervention is youth focused. Most of the efforts have been to ensure that the youth becomes engaged in services. Less attention was paid to family issues, particularly at the outset of service delivery. It may be that expanding the program to include more of a family focus might be indicated (27). It also may be that the needs of caregivers are often not identified at the initiation of services. Parents struggling with their child's problems may be less open to discussing their own difficulties. Perhaps as the liaisons become more involved with these families the needs of the caregivers become more apparent.
This study had a number of limitations. First, all the data came from the service providers. No direct assessments of the youths or their families were undertaken. However, the CANS-MH is audited annually at each site, which ensures the reliability with which it is completed. Second, follow-up was only for the duration of the intervention. We do not know whether the impact of the intervention lasts beyond the involvement of the liaison with the youth and his or her family. Third, no comparison or control group was available to assess whether the observed outcomes were attributable to the intervention or to other factors operating in these youths' lives. However, the observed rearrest rate for MHJJ youths is substantially below the statewide rate of 72 percent of youths arrested and placed in detention; the rearrest rate for successfully linked MHJJ youths was even lower. Regardless, confirmation of the effectiveness of this intervention would require a carefully controlled randomized clinical trial. Finally, there have been notable differences in the speed and success of implementation of the intervention in different settings. Building on the work on organizational aspects of service delivery (28,29), we plan to explore site differences.
Conclusions
The initial findings from the Illinois Mental Health Juvenile Justice initiative suggest that the four evaluation questions outlined above can all be answered in the affirmative. Youths with affective and psychotic disorders can be identified while in detention. These youths can be linked to community-based mental health services. This linkage is associated with improvements in mental health. Improved mental health is associated with reduced likelihood of rearrest. With a relatively inexpensive intervention that capitalizes on existing community-based services, youths in the juvenile justice system who have specific mental health needs can be served effectively.
Dr. Lyons, Dr. Griffin, and Dr. Shasha are affiliated with the mental health services and policy program of Northwestern University Feinberg School of Medicine, 710 North Lake Shore Drive, Abbott 1206, Chicago, Illinois (e-mail, [email protected]). Dr. Griffin is also with the Illinois Office of Mental Health in Chicago, with which Ms. Quintenz is affiliated. Dr. Jenuwine is with the Indiana University School of Law in Bloomington.
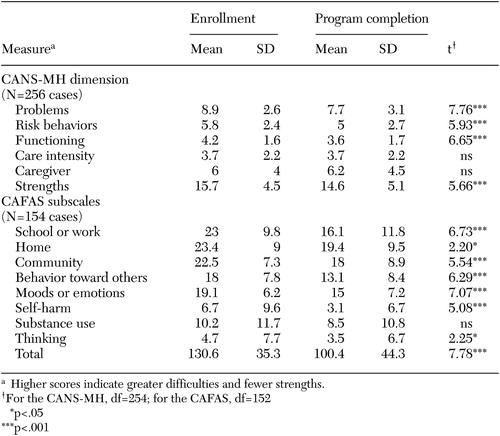 |
Table 1. Mean±SD scores on dimensions of the Child and Adolescent Needs and Strengths—Mental Health Scale (CANS-MH) and subscales of the Child and Adolescent Functional Assessment Scale (CAFAS) at enrollment and at the end of the service episode
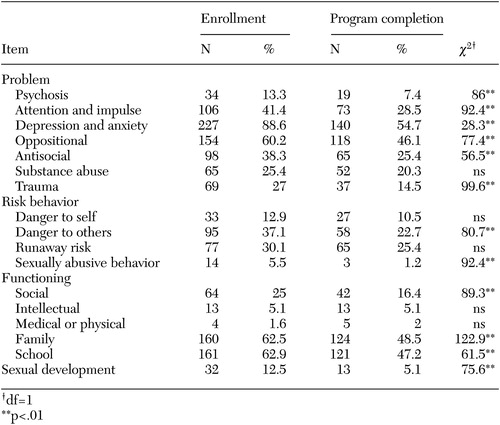 |
Table 2. Proportions of youths with ratings indicating a need for services (2 or 3) on individual problem, risk behavior, and functioning items of the Child and Adolescent Needs and Strengths-Mental Health Scale at enrollment and program completion (N=256 cases)
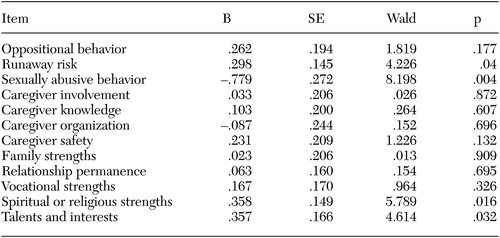 |
Table 3. Results of logistic regression analysis to predict rearrest by using items of the Child and Adolescent Needs and Strengths-Mental Health Scale at program enrollment (N=314 youths)
1. Steiner H, Cauffman E: Juvenile justice, delinquency, and psychiatry. Child and Adolescent Psychiatric Clinics of North America 7:653–672, 1998Crossref, Medline, Google Scholar
2. Lyons JS, Baerger DR, Quigley P, et al: Mental health service needs of juvenile offenders: a comparison of detention, incarceration, and treatment settings. Children's Services: Social Policy, Research, and Practice 4:69–85, 2001Crossref, Google Scholar
3. Teplin LT, Abrams KM, McClelland GM, et al: Psychiatric disorders in youth in juvenile detention. Archives of General Psychiatry 59:1133–1143, 2002Crossref, Medline, Google Scholar
4. Snyder HN: Juvenile Arrests, 1999. Washington, DC, Office of Juvenile Justice and Delinquency Prevention, 2000Google Scholar
5. Griffin G, Jenuwine M: Using therapeutic jurisprudence to bridge the juvenile justice and mental health systems. University of Cincinnati Law Review 70:1–23, 2002Google Scholar
6. Henggeler SW, Rowland MD, Pickrel SG, et al: Investigating family-based alternatives to institution-based mental health services for youth: lessons learned from the pilot study of a randomized field trial. Journal of Clinical Child Psychology 26:226–233, 1997Crossref, Medline, Google Scholar
7. Bourduin CM, Schaeffer CM: Multisystemic treatment of juvenile sexual offenders: a progress report. Journal of Psychology and Human Sexuality 13:25–42, 2001Crossref, Google Scholar
8. Letourneau EJ, Cunningham PB, Henggeler SW: Multisystemic treatment of antisocial behavior in adolescents, in Treating Chronic and Severe Mental Disorders: A Handbook of Empirically Supported Interventions. Edited by Hofmann SG, Thompson MC. New York, Guilford, 2002Google Scholar
9. Wolff N: Courts as therapeutic agents: thinking past the novelty of mental health courts. Journal of the American Academy of Psychiatry and the Law 30:431–437, 2002Medline, Google Scholar
10. Stroul BA: Systems of Care for Children and Adolescents With Severe Emotional Disturbances: What Are the Results? Washington, DC, Georgetown University Child Development Center, 1993Google Scholar
11. Stroul B, Friedman R: A System of Care for Children and Youth With Severe Emotional Disturbances, rev ed. Washington, DC, Georgetown University Child Development Center, National Technical Assistance Center for Children's Mental Health, 1986Google Scholar
12. Stroul B, Friedman R: The system of care concept and philosophy, in Children's Mental Health: Creating Systems of Care in a Changing Society. Baltimore, Brookes, 1996Google Scholar
13. US Surgeon General: Report of the United States Surgeon General's Conference on Children's Mental Health: A National Action Agenda. Washington, DC, Department of Health and Human Services, 2001Google Scholar
14. Rawal P, Romansky J, Jenuwine M, et al: Racial differences in the mental health needs and service utilization in the juvenile justice system. Journal of Behavioral Health Services and Research, in pressGoogle Scholar
15. Scott MA, Snowden L, Libby AM: From mental health to juvenile justice: what factors predict this transition? Journal of Child and Family Studies 11:299–311, 2002Google Scholar
16. Kaplan G, Pannullo D, Brodzinsky D, et al: Noncompliance with family court mandated evaluations in a juvenile justice clinic. Bulletin of the American Academy of Psychiatry and the Law 22:31–38, 1995Google Scholar
17. Diagnostic and Statistical Manual of Psychiatric Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
18. Lyons JS: The Severity and Acuity of Psychiatric Illness, Child and Adolescent Version. San Antonio, Tex, Psychological Corporation, 1998Google Scholar
19. Leon SC, Lyons JS, Uziel-Miller ND, et al: Evaluating the use of psychiatric hospitalization by residential treatment. Journal of the American Academy of Child and Adolescent Psychiatry 39:1496–1501, 2001Crossref, Google Scholar
20. Leon SC, Uziel-Miller ND, Lyons JS, et al: Psychiatric hospital utilization of children and adolescents in state custody. Journal of the American Academy of Child and Adolescent Psychiatry 38:305–310, 1999Crossref, Medline, Google Scholar
21. Lyons JS, Weiner DA, Lyons MB: Measurement as Communication: The Child and Adolescent Needs and Strengths for Children With Mental Health Challenges. Working paper. Winnetka, Ill, Buddin Praed Foundation, 2003Google Scholar
22. Anderson RL, Lyons JS, Giles DM, et al: Examining the reliability of the Child and Adolescent Needs and Strengths-Mental Health (CANS-MH) Scale from two perspectives: a comparison of clinician and researcher ratings. Journal of Child and Family Studies, in pressGoogle Scholar
23. Hodges K, McKnew D, Cytryn L, et al: The Child Assessment Schedule (CAS) diagnostic interview: a report on reliability and validity. Journal of the American Academy of Child and Adolescent Psychiatry 21:468–473, 1982Crossref, Google Scholar
24. Hodges K, Wotring J: Client typology based on functioning across domains using the CAFAS: implications for service planning. Journal of Behavioral Health Services and Research 27:257–270, 2000Crossref, Medline, Google Scholar
25. Lyons JS, Rawal P, Yeh I, et al: Use of measurement audit in outcomes management. Journal of Behavioral Health Services and Research 29:75–80, 2002Crossref, Medline, Google Scholar
26. Olson D, Dooley B: Report to the Illinois Criminal Justice Information Authority. White paper. Springfield, Ill, 2003Google Scholar
27. Woolfenden SR, Williams K, Peat JK: Family and parenting interventions for conduct disorder and delinquency: a meta-analysis of randomized controlled trials. Archives of Diseases in Childhood 86:251–256, 2002Crossref, Medline, Google Scholar
28. Glisson C: Structure and technology in human service organizations, in Human Services as Complex Organizations. Edited by Hasenfeld Y. Newbury Park, Calif, Sage, 1992Google Scholar
29. Scott WR: Organizations: Rational, Natural, and Open Systems, 3rd ed. Englewood Cliffs, NJ, Prentice Hall, 1992Google Scholar