Evaluation of a Model of Violence Risk Assessment Among Forensic Psychiatric Patients
Abstract
OBJECTIVE: This study tested the interrater reliability and criterion-related validity of structured violence risk judgments made by using one application of the structured professional judgment model of violence risk assessment, the HCR-20 violence risk assessment scheme, which assesses 20 key risk factors in three domains: historical, clinical, and risk management. METHODS: The HCR-20 was completed for a sample of 100 forensic psychiatric patients who had been found not guilty by reason of a mental disorder and were subsequently released to the community. Violence in the community was determined from multiple file-based sources. RESULTS: Interrater reliability of structured final risk judgments of low, moderate, or high violence risk made on the basis of the structured professional judgment model was acceptable (weighted kappa=.61). Structured final risk judgments were significantly predictive of postrelease community violence, yielding moderate to large effect sizes. Event history analyses showed that final risk judgments made with the structured professional judgment model added incremental validity to the HCR-20 used in an actuarial (numerical) sense. CONCLUSIONS: The findings support the structured professional judgment model of risk assessment as well as the HCR-20 specifically and suggest that clinical judgment, if made within a structured context, can contribute in meaningful ways to the assessment of violence risk.
Literally dozens of clinical and legal settings call for violence risk assessment and management by mental health professionals (1,2). One example is release from forensic psychiatric hospitalization, the setting of the study reported in this article.
A prominent development in the risk assessment field has been the focus of research on instrumentation and models of decision making (3,4,5,6,7). Two traditional methods for making decisions—clinical and actuarial models—have been discussed in the medical and behavioral sciences literatures (8,9,10) and have been applied to violence risk assessment. The clinical method has been described as an "informal, 'in the head,' impressionistic, subjective conclusion, reached (somehow) by a human clinical judge" (9). In contrast, the actuarial method has been described as "a formal method" that "uses an equation, a formula, a graph, or an actuarial table to arrive at a probability, or expected value, of some outcome" (9).
Some consensus exists among commentators that sole reliance on unstructured clinical decision making is inadequate for conducting risk assessments (11). Actuarial prediction methods have been applied to samples of psychiatric patients and have achieved high levels of statistical accuracy (4,5,12). Despite this achievement, commentators (11,13,14,15,16,17,18,19,20,21,22,21,24) have noted potential shortcomings associated with strict actuarial models of prediction, including potential lack of generalizability and applicability beyond samples of development; difficulty of replicating clinical reality by using actuarial methods; tendency of actuarial methods to exclude potentially important risk factors; rigidity and lack of sensitivity to change; and failure optimally to inform violence prevention and risk management.
Another research-based model of risk assessment—structured professional judgment—uses a professional guideline approach to decision making (14,17,18,19,22). Several sets of professional guidelines have been developed under the structured professional judgment approach (3,6,25,26,27), including the HCR-20 violence risk assessment scheme (6), so named for its 20 risk factors in three domains—historical, clinical, and risk management. In structured professional judgment risk assessment, evaluators review all relevant clinical data to determine the presence of specific risk factors, which themselves are included (defined and operationalized) in professional manuals on the basis of their association with violence in the scientific and professional literatures. On the basis of these factors, an overall judgment of risk is made, referred to here as the structured final risk judgment.
Although there are no fixed guidelines about how risk factors are combined to reach an overall judgment, structure is imposed on the decision-making process in several ways: specifying a list of empirically supported risk factors, operationalizing these risk factors, providing fixed scoring guidelines for the factors, and providing some guidance for making final decisions of low, moderate, or high risk (again, the structured final risk judgment). A key assumption underlying the structured professional judgment approach is that professional discretion is potentially valuable and appropriate for the assessment of risk, although a degree of structure is necessary to reduce the complexity of the clinical task and guide the exercise of discretion.
There are several steps in the validation of the structured professional judgment model and its specific instruments (14), including establishing whether the risk factors chosen for inclusion in schemes can be scored reliably and whether they actually relate to violence. A fair amount of research has been published on this topic—a series of research studies has established the interrater reliability of evaluators' judgments about the presence of various risk factors as well as the validity of the judgments in both retrospective and prospective studies (12,28,29,30,31,32,33,34,35,36,37,38,39).
However, few studies have examined the reliability or validity of the structured final risk judgments made under the structured professional judgment model (35,40), despite the fact that these judgments represent the central intended clinical use of these measures. In the existing measures, structured final risk judgments of low, moderate, or high risk typically are made according to the likelihood of violence and the degree of intervention the case will require. The ratings reflect not only the presence of risk factors but also their perceived relevance, interactions among them, and the likelihood that they will be managed effectively through monitoring, treatment, supervision, and victim safety enhancement. Such overall judgments are critically important in clinical decisions about such matters as case prioritization and intervention.
In this study, we evaluated the structured final risk judgments made on the basis of the HCR-20 violence risk assessment scheme (6), which is the structured professional judgment measure about which the most research has been published. We had three research questions. First, can HCR-20 items, scales, and—particularly—structured final risk judgments be made with acceptable interrater reliability? Second, are HCR-20 items, scales, and—particularly—structured final risk judgments associated with future violence? Finally, what is the incremental validity of structured final risk judgments with respect to actuarial (arithmetic) combinations of HCR-20 item ratings?
To address these questions, we conducted a pseudo-prospective community follow-up study of 100 forensic psychiatric patients. The design was pseudo-prospective in the sense that predictive measures—that is, the HCR-20 items and judgments—were completed on the basis of information available at discharge (1996 to 1997), although the actual research coding was done later (2000-2001). The follow-up period occurred later (from discharge up to 2001) than the time frame for coding the HCR-20. This approach is common to risk assessment research (5,12).
Methods
Study participants
The sample consisted of 100 forensic psychiatric patients who were found not guilty by reason of a mental disorder and who subsequently had one or more release hearings. The participants were drawn from a larger, ongoing prospective study of the predictive validity of the HCR-20. The larger study of 175 patients uses version 1 of the HCR-20 (41) and does not include the structured final risk judgments. Several preliminary reports of data from the larger study have been made (42,43,44). From 116 of 175 patients who were released from hospitalization in the period 1996 to 1997 (the study period), 100 were randomly selected to serve as participants in the study reported here. The remaining 16 patients participated in piloting and training activities. The study was approved by the institutional review board of Simon Fraser University.
In the sample of 100, most participants were male (91 percent), did not have children (30 percent), and were unmarried (67 percent). A majority of the patients were unemployed (93 percent). Less than half (40 percent) had completed high school. Most (92 percent) had a previous violence charge, 48 had a previous violence conviction, a majority (79 percent) had a current violent index offense, and many (34 percent) had a juvenile record. A majority (96 percent) had previously received psychiatric treatment, including inpatient treatment (83 percent). Primary diagnoses were schizophrenia (73 percent), mood disorders (18 percent), substance-related disorders (5 percent), and other (3 percent). A quarter of the sample (24 percent) had a diagnosis of a personality disorder.
Procedure
HCR-20 (version 2). The HCR-20 comprises 20 key risk factors in three domains—historical, clinical, and risk management, which are listed in Table 1. The historical domain reflects factors related to past conduct, mental disorder, and social adjustment, which typically are documented or established in official records. The clinical domain reflects factors related to current psychological functioning, which typically are observed or inferred from recent behavior. The risk management domain reflects factors related to future adjustment problems, which are speculated or anticipated on the basis of historical and clinical factors as well as plans and goals.
As recommended in the test manual, the 20 items were rated 0, absent; 1, possibly or partially present; or 2, definitely present. As is commonly done for research, we summed the numerical item ratings to yield four dimensional scores: historical scores, clinical scores, risk management scores, and HCR-20 total scores (all items). Thus possible HCR-20 total scores ranged from 0 to 40. Raters then made structured final risk judgments of 1, low; 2, moderate; or 3, high (explained in further detail in the manual). Several other ratings were used as covariates in some analyses—for example, confidence ratings and whether HCR-20 items were considered to be "critical" or "criminogenic." A rating of critical indicates that the raters believed that the item could, on its own, compel a rating of high risk (27). A rating of criminogenic indicates that the raters believed the items in the case at hand were relevant to risk of violence.
The raters were two master's-level clinicians and clinical psychology graduate students. This small number of raters was chosen to minimize rater effects. Both raters had clinical experience in psychiatric, correctional, and forensic settings; had completed core courses in clinical psychology and forensic mental health; and were trained specifically to use the HCR-20, including completion of three sample cases. After training, the raters independently completed the HCR-20 for five individuals who had been acquitted by reason of a mental disorder and resolved difficulties with the trainer. The raters gathered clinical information from the full clinical-legal files of participants as they existed at the time of discharge. The files were rich and detailed, containing social, psychological, psychiatric, medical, criminal, and legal information. Each rater assessed 75 participants, with an overlap of 50 percent—one rater coded participants 1 through 75 and the other coded participants 26 through 100, so that participants 26 through 75 were coded twice, for interrater reliability. This training and coding procedure is representative of HCR-20 research and consistent with the manual.
Detection of violence. Violence in the community was coded both on the basis of criminal records of convictions and from clinical files after discharge from the hospital by separate raters who were blinded to HCR-20 ratings. Clinical files were based primarily on outpatient forensic psychiatric, psychological, and nursing contacts, usually conducted at regularly scheduled intervals—for example, monthly. However, clinicians were not part of data collection, so standardized violence interviewing procedures were not possible. The clinical files included reports from patients, families, and treating professionals during the course of the follow-up. Thus, although only two file-based sources were used to detect violence, one of these included self-reports and collateral reports. In accordance with the HCR-20 manual, violence was defined as actual, attempted, or threatened physical harm of another person. Acts of violence were divided into broad categories of any violence, physical violence, and nonphysical violence, which is consistent with the approaches used in other risk assessment research (12,45,46,47).
Statistical analyses
Intraclass correlations (ICCs) were used for reliability analyses. The ICC is a measure of chance-corrected agreement rather than association (such as Pearson's r) and hence is sensitive to additive and multiplicative biases between raters (48). ICC is mathematically equivalent to a weighted kappa (49,50).
To address validity analyses, several statistical procedures were used, including receiver operating characteristic (ROC) analysis (51). ROC analysis is independent of the criterion base rate and produces an effect—the area under the curve (AUC)—by plotting sensitivity and specificity pairs for each possible cutoff score on a measure. The AUC equals the probability that a violent person will receive a higher score on the predictor than a nonviolent person.
Survival analysis was used to evaluate whether HCR-20 structured final risk judgments added incrementally to numerical scores. This analysis uses time to an event as the dependent measure, models the time to an event, and controls for unequal follow-up times between participants (52).
All statistical analyses were conducted with use of SPSS, version 10.1 (53).
Results
Descriptive variables
The mean±SD total HCR-20 score of the 100 patients in our sample was 24.70±4.64, and the range was 11 to 36. For the historical scale, the mean was 14.14±2.79 (range, 6 to 19); for the clinical scale, 4.68±2.02 (range, 0 to 10), and for the risk management scale, 5.88±1.49 (range, 2 to 9). The proportions of patients who were violent after release were 14 percent for nonphysical violence, 15 percent for physical violence, and 22 percent for any violence. The average time from release to follow-up was 42.91±13.29 months (median, 45.27 months; range, .13 to 63.07 months).
Reliability
The ICCs of the two raters for the HCR-20 items and scales, based on the 50 overlapping patients, are listed in Table 1. A one-way random-effects model of the ICC was used for both the reliability of single-rater ratings (ICC1) and averaged ratings (ICC2). ICC1 was considered the primary index of reliability, but ICC2 was used to gauge the potential reliability of averaged ratings. For individual historical items, ICC1 ranged from .41 (historical scale, item 4) to 1.0 (historical scale, item 7). Because the latter item reflected mere transcription of preexisting psychopathy scores (54), item 8 on the historical scale attained the highest actual interrater reliability (ICC1=.89). Most ICC1 values (eight of ten) were equal to or greater than .70. ICC2 values paralleled this pattern, but, as expected, were higher. Most ICC2 values (eight of ten) were equal to or greater than .80. ICC1 values for the clinical scale ranged from .34 (item five) to .69 (item 3). None of the values was greater than .70. Items on the risk management scale were problematic; ICC1 values ranged from .01 (item 5) to .54 (item 3). None of the values was greater than .60.
Agreement for the structured final risk judgments is summarized in Table 2. The two raters agreed in the case of 35 (70 percent) of the 50 overlapping patients, and there were no "low/high-risk" errors. Chance-corrected agreement (ICC1, or weighted kappa) was .61, (p≤.001, 95 percent confidence interval [CI]=.41 to .76); ICC2 was .76 (p≤.001, CI=.58 to .86).
Validity
The proportions of each type of violence across structured final risk judgments of low, moderate, and high risk are shown in Table 3. These judgments were related to each type of violence. AUC values from ROC analyses for these HCR-20 clinical judgments were statistically significant for each outcome criterion, as can be seen from Table 4. AUCs for the HCR-20 structured final risk judgments varied between .68 and .74, depending on the violence index.
Kaplan-Meier bivariate survival analysis was conducted for each outcome criterion. When "any violence" was used as the dependent measure, structured final risk judgments emerged as a significant predictor (log rank=21.1, p<.001). Results were similar when "physical violence" was used as the outcome (details can be obtained from the first author). The survival function is shown in Figure 1, illustrating that patients who were judged to be high risk were more likely to be violent—and to be violent sooner—than other patients.
Multivariate analyses
Cox regression analyses were carried out with use of "any violence" as the outcome. The results were highly similar for physical violence. First, scores on the historical, clinical, and risk management scales were directly entered as block 1. On block 2, the HCR-20 structured final risk judgments were entered by using the forward conditional method. This entry procedure was used so that all the HCR-20 numerical scores were included in the final model but that HCR-20 structured final risk judgments would be included only if they significantly improved the overall model.
The results are presented in Table 5. When "any violence" was used as the outcome measure, the historical, clinical, and risk management scores together produced a significant model fit on block 1 (-2 log likelihood=181.754, χ2=9.904, df=3, p≤.05). Only the clinical scale was a significant predictor in the model. The HCR-20 structured final risk judgments were then entered as block 2 and produced a significant improvement to the model's fit (χ2 change=9.828, df=1, p≤.01). The HCR-20 structured final risk judgments were most strongly related to violence, over and above the actuarial scores.
Analyses were conducted that also added potentially relevant covariates to block 1 of the Cox regression model: psychopathy score on the Psychopathy Checklist-Revised (PCL-R) (54), gender, violent index offense, critical item summation, criminogenic item summation, and numerical confidence (scored 1 to 10). This initial block was not significant, although the clinical domain was (-2 log likelihood=178.556, χ2=12.276, df=9, p=.20). This result probably stemmed from lower power associated with a higher number of predictors. Use of a forward conditional (stepwise) entry procedure resulted in a significant overall model, because fewer variables entered the overall model. The addition of the structured final risk judgments as the second block improved the model's fit (χ2 change=9.615, df=2, p≤.01). Only the structured final risk judgments were significant in the final model. As such, these analyses show that structured final risk judgments—or clinical judgments—added incrementally to not only numerical HCR-20 scores but also to other potential predictors as well, used actuarially.
Discussion
Actuarial and structured professional judgment models of risk assessment have been developed in response to unstructured clinical prediction. In this study we sought to evaluate the HCR-20 generally and to evaluate one aspect of the HCR-20 and the structured professional judgment model specifically—that is, the model's structured final risk judgments intended for use by clinicians. Bivariate analysis showed that such judgments predicted violence with moderate to large statistical effects. That is, AUC values from .68 to .74, converted into Cohen's d with transformational procedures provided by Dunlap (55) and on the basis of Cohen's (56) suggestions for guidance regarding the size of effects (d≥.80 is considered large), suggested that these AUCs were moderate to large. Importantly, the judgments added incrementally to models consisting of HCR-20 numerical indexes and to models including other potentially important covariates. These validity findings based on the HCR-20 are consistent with those of studies of other structured professional judgment measures (35,41).
Interrater reliability of structured final risk judgments (.61 and .76) was "good" (49) to "substantial" (50), without instances of low/high-risk disagreements between raters. These findings also parallel those of others (35), who reported ICC values of .57 to .61 for structured final risk judgments with use of another measure (27). Some authors have warned against the use of clinical judgments in risk assessment (5,9) and clinical decision making more generally (10,57,58,59). The study reported here, along with other research (35,40), suggests that this "lack of utility" position ought to be revisited with respect to structured clinical decisions made on the basis of the structured professional judgment model of risk assessment. This model addresses some of the concerns about unstructured clinical judgment, such as subjectivity, lack of attention to important risk factors, and variability across clinicians. It also has been shown in three of three direct comparisons (including in this study) to be more strongly related than actuarial predictions to relevant outcome criteria (35,40).
Limitations of this study include its pseudo-prospective design and use of ratings based solely on data obtained from patients' files. It is likely that both of these factors limited reliability and validity, because they precluded optimal measurement procedures, the specific targeting of study constructs by raters, and they necessitate reliance on the clinical reporting of other professionals. However, in this study file-based clinical information included numerous richly descriptive psychiatric, psychological, social work, nursing, legal, and other reports and documents. Furthermore, the design is a reasonable alternative to a true prospective design if raters are kept blinded, because it permits statements to be made about the relationship between predictors and subsequently occurring criteria.
Another limitation was the use of only two raters. This approach was used to minimize substantial rater effects. However, subsequent research will need to address such possible effects—for example, does the rater's gender or race matter? Our study was considered a prerequisite to these other necessary efforts. Furthermore, the relationship between numerical HCR-20 ratings and violence, although statistically significant (in the case of total HCR-20 scores and clinical scores , was smaller than in some previous HCR-20 studies (12).
Whether our findings would be replicated if the numerical findings were stronger is an empirical question. Another important question is whether the findings would be generalizable if more serious forms of violence could be measured (4). The results of our study were similar whether physical (more serious) or nonphysical (less serious) violence was used as a criterion. Similar findings have been reported for other HCR-20 studies (12).
Measures were coded for research purposes, so HCR-20 scores did not follow the patients. However, the treating psychiatrists probably would have included an HCR-20 completed independently for clinical practices, or a risk assessment of some kind, in their discharge summaries. It is unclear what, if any, effect this practice would have on the validity of the HCR-20 indexes collected in this study for research purposes. A higher HCR-20 score could cause increased surveillance, leading to observation of more violence. It also reasonably could lead to more effective risk management and treatment, leading to fewer episodes of violence to observe. Whatever the effect, it was indirect because the outpatient clinicians did not have the HCR protocols used in this study.
Conclusions
The results of this study provide reasonable support for the decision-making scheme of the structured professional judgment model of risk assessment and are inconsistent with the position that clinical decisions about violence risk are perforce unreliable and invalid. The study evaluated one piece of the structured professional judgment model. Subsequent studies should consider whether use of the structured professional judgment model actually prevents subsequent violence—an explicit goal of the structured professional judgment model (13,14,17,18,19) and an emerging conceptual theme in the field more broadly (15,60,61). That is, the structured professional judgment model intends to guide clinicians to arrive at a risk level through consideration of what risk factors are present, their salience for the individual at hand, and the attendant risk management and intervention strategies that will reduce these factors.
Acknowledgments
The authors thank Jodi Viljoen and Steph Griffiths for their research assistance. They also thank Christopher D. Webster, Ph.D., and Derek Eaves, M.B., Ch.B., who along with Dr. Hart received a grant from the British Columbia Health Research Foundation that funded the original study from which the participants in this study were selected.
Dr. Douglas is affiliated with the department of mental health law and policy of the Florida Mental Health Institute at the University of South Florida, 13301 Bruce B. Downs Boulevard, Tampa, Florida 33612 (e-mail, [email protected]). He is also affiliated with Mid-Sweden University in Sundsvall, Sweden. Dr. Ogloff is with the School of Psychology, Psychiatry, and Psychological Medicine at Monash University in Melbourne, Australia, and with the Victorian Institute of Forensic Mental Health in Fairfield, Australia. Dr. Hart is with the department of psychology at Simon Fraser University in Burnaby, British Columbia, Canada.
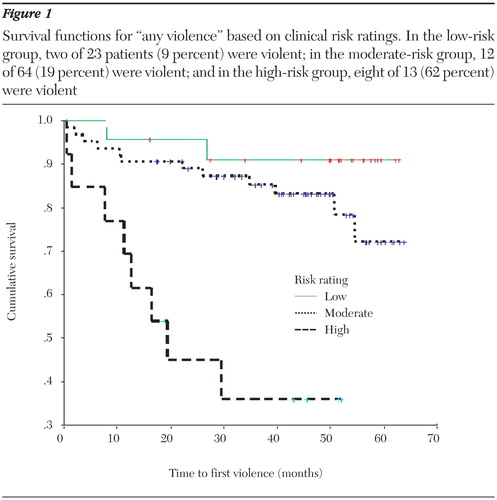
Figure 1. Survival functions for "any violence" based on clinical risk ratings. In the low-risk group, two of 23 patients (9 percent) were violent; in the moderate-risk group, 12 of 64 (19 percent) were violent; and in the high-risk group, eight of 13 (62 percent) were violent
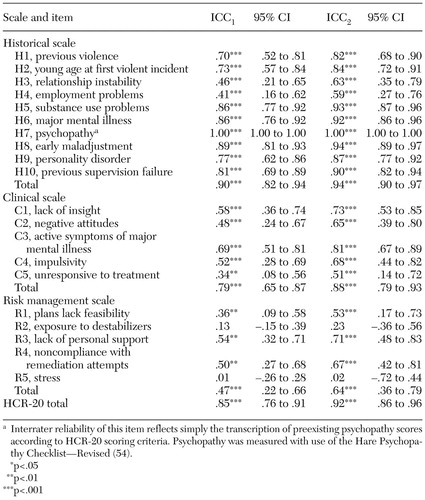 |
Table 1. Interrater reliability (ICC1 and ICC2) of two raters for HCR-20 items and scales for 50 forensic psychiatric patients
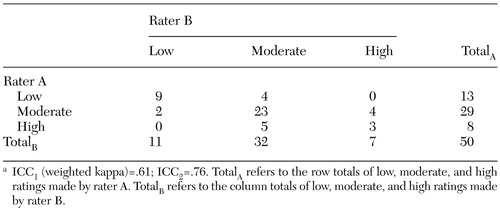 |
Table 2. Agreement between two raters on structured final risk judgments for 50 forensic psychiatric patientsa
a ICC1 (weighted kappa)=.61; ICC2=.76. TotalA refers to the row totals of low, moderate, and high ratings made by rater A. TotalB refers to the column totals of low, moderate, and high ratings made by rater B.
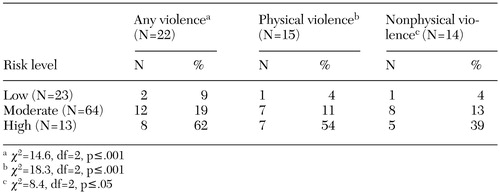 |
Table 3. Postrelease violence across levels of structured final risk judgments for 100 forensic psychiatric patients
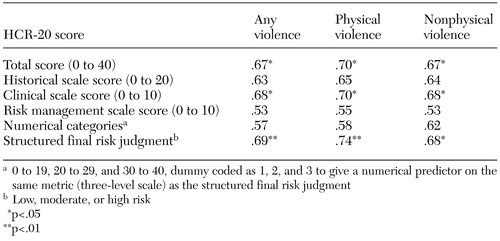 |
Table 4. Area under the receiver operating characteristic curves for HCR-20 scores for a sample of 100 forensic psychiatric patients
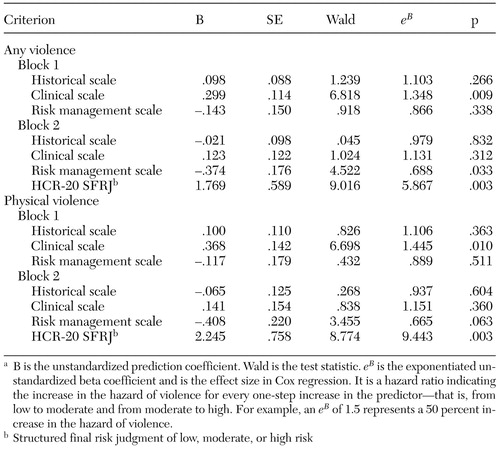 |
Table 5. Cox regression analyses comparing actuarial and structured (clinical) final risk judgments for a sample of 100 forensic psychiatric patientsa
a B is the unstandardized prediction coefficient. Wald is the test statistic. eB is the exponentiated unstandardized beta coefficient and is the effect size in Cox regression. It is a hazard ratio indicating the increase in the hazard of violence for every one-step increase in the predictor—that is, from low to moderate and from moderate to high. For example, an eB of 1.5 represents a 50 percent increase in the hazard of violence.
1. Shah SA: Dangerousness and mental illness: some conceptual, prediction, and policy dilemmas, in Dangerous Behavior: A Problem in Law and Mental Health. Edited by Frederick C. Washington, DC, Government Printing Office, 1978Google Scholar
2. Lyon DR, Hart SD, Webster CD: Violence risk assessment, in Law and Psychology: Canadian Perspectives. Edited by Schuller R, Ogloff JRP. Toronto, University of Toronto Press, 2001Google Scholar
3. Borum R, Bartel P, Forth A: Manual for the Structured Assessment for Violence Risk in Youth (SAVRY): Consultation Version. Tampa, Fla, University of South Florida, Florida Mental Health Institute, 2002Google Scholar
4. Monahan J, Steadman HJ, Silver E, et al: Rethinking Risk Assessment: The MacArthur Study of Mental Disorder and Violence. New York, Oxford University Press, 2001Google Scholar
5. Quinsey VL, Harris GT, Rice M, et al: Violent Offenders: Appraising and Managing Risk. Washington, DC, American Psychological Association, 1998Google Scholar
6. Webster CD, Douglas KS, Eaves D, et al: HCR-20: Assessing Risk for Violence, Version 2. Burnaby, BC, Canada, Simon Fraser University, Mental Health, Law, and Policy Institute, 1997Google Scholar
7. Heilbrun K, Rogers R, Otto R: Forensic assessment: current status and future directions, in Psychology and Law: Reviewing the Discipline. Edited by Ogloff JRP. New York, Kluwer, 2001Google Scholar
8. Meehl PE: Clinical Versus Statistical Prediction. Minneapolis, University of Minnesota Press, 1954Google Scholar
9. Grove WM, Meehl PE: Comparative efficiency of informal (subjective, impressionistic) and formal (mechanical, algorithmic) prediction procedures: the clinical-statistical controversy. Psychology, Public Policy, and Law 2:293–323, 1996Crossref, Google Scholar
10. Grove WM, Zald DH, Lebow BS, et al: Clinical versus mechanical prediction: a meta-analysis. Psychological Assessment 12:19–30, 2000Crossref, Medline, Google Scholar
11. Melton GB, Petrila J, Poythress NG, et al: Psychological Evaluations for the Courts: A Handbook for Mental Health Professionals and Lawyers, 2nd ed. New York, Guilford, 1997Google Scholar
12. Douglas KS, Ogloff JRP, Nicholls TL et al: Assessing risk for violence among psychiatric patients: the HCR-20 violence risk assessment scheme and the Psychopathy Checklist: Screening Version. Journal of Consulting and Clinical Psychology 67:917–930, 1999Crossref, Medline, Google Scholar
13. Douglas KS, Cox DN, Webster CD: Violence risk assessment: science and practice. Legal and Criminological Psychology 4:149–184, 1999Crossref, Google Scholar
14. Douglas KS, Kropp PR: A prevention-based paradigm for violence risk assessment: clinical and research applications. Criminal Justice and Behavior 29:617–658, 2002Crossref, Google Scholar
15. Dvoskin JA, Heilbrun K: Risk assessment and release decision-making: toward resolving the great debate. Journal of the American Academy of Psychiatry and the Law 29:6–10, 2001Medline, Google Scholar
16. Grubin D: Predictors of risk in serious sex offenders. British Journal of Psychiatry 170:S17-S21, 1997Google Scholar
17. Hart SD: The role of psychopathy in assessing risk for violence: conceptual and methodological issues. Legal and Criminological Psychology 3:121–137, 1998Crossref, Google Scholar
18. Hart SD: Assessing and managing violence risk, in HCR-20 Violence Risk Management Companion Guide. Edited by Douglas KS, Webster CD, Hart SD, et al. Burnaby, BC, Simon Fraser University, Mental Health Law and Policy Institute, and Tampa, Fla, Department of Mental Health Law and Policy, University of South Florida, 2001Google Scholar
19. Hart SD: Complexity, uncertainty, and the reconceptualization of risk assessment. Available at www.sfu.ca/psychology/groups/faculty/hart, 2001Google Scholar
20. Litwack TR: Actuarial versus clinical assessments of dangerousness. Psychology, Public Policy, and Law 7:409–443, 2001Crossref, Google Scholar
21. Litwack TR, Schlesinger LB: Dangerousness risk assessments: research, legal, and clinical considerations, in Handbook of Forensic Psychology, 2nd ed. Edited by Hess AK, Weiner IB. New York, Wiley, 1999Google Scholar
22. Otto RK: Assessing and managing violence risk in outpatient settings. Journal of Clinical Psychology 56:1239–1262, 2000Crossref, Medline, Google Scholar
23. Reed J: Risk assessment and clinical risk management: the lessons from recent inquiries. British Journal of Psychiatry 170:S4-S7, 1997Google Scholar
24. Snowden P: Practical aspects of clinical risk assessment and management. British Journal of Psychiatry 170:S32-S34, 1997Google Scholar
25. Augimeri LK, Koegl CJ, Webster, CD, et al: Early Assessment Risk List for Boys (EARL-20B), version 2. Toronto, Earlscourt Child and Family Centre, 2001Google Scholar
26. Boer DP, Hart SD, Kropp, PR, et al: Manual for the Sexual Violence Risk—20: Professional Guidelines for Assessing Risk of Sexual Violence. Vancouver, British Columbia Institute Against Family Violence, 1997Google Scholar
27. Kropp PR, Hart SD, Webster CD, et al: Manual for the Spousal Assault Risk Assessment Guide, 3rd ed. Toronto, Multi-Health Systems, 1999Google Scholar
28. Belfrage H: Implementing the HCR-20 scheme for risk assessment in a forensic psychiatric hospital: integrating research and clinical practice. Journal of Forensic Psychiatry 9:328–338, 1998Crossref, Google Scholar
29. Belfrage H, Fransson G, Strand S: Prediction of violence using the HCR-20: a prospective study in two maximum-security correctional institutions. Journal of Forensic Psychiatry 11:167–175, 2000Crossref, Google Scholar
30. Dernevik M, Grann M, Johansson S: Violent behaviour in forensic psychiatric patients: risk assessment and different risk management levels using the HCR-20. Psychology, Crime, and Law 8:93–111, 2002Crossref, Google Scholar
31. Doyle M, Dolan M, McGovern J: The validity of North American risk assessment tools in predicting in-patient violent behaviour in England. Legal and Criminological Psychology 7:141–154, 2002Crossref, Google Scholar
32. Douglas KS, Webster CD: The HCR-20 violence risk assessment scheme: concurrent validity in a sample of incarcerated offenders. Criminal Justice and Behavior 26:3–19, 1999Crossref, Google Scholar
33. Grann M, Belfrage H, Tengström A: Actuarial assessment of risk for violence: predictive validity of the VRAG and the historical part of the HCR-20. Criminal Justice and Behavior 27:97–114, 2000Crossref, Google Scholar
34. Kroner DG, Mills JF: The accuracy of five risk appraisal instruments in predicting institutional misconduct and new convictions. Criminal Justice and Behavior 28:471–489, 2001Crossref, Google Scholar
35. Kropp PR, Hart SD: The Spousal Assault Risk Assessment (SARA) Guide: reliability and validity in adult male offenders. Law and Human Behavior 24:101–118, 2001Crossref, Google Scholar
36. Strand S, Belfrage H, Fransson G, et al: Clinical and risk management factors in risk prediction of mentally disordered offenders: more important that actuarial data? Legal and Criminological Psychology 4:67–76, 1999Google Scholar
37. Buchanan A: Review of the book HCR-20: Assessing Risk for Violence, version 2. Criminal Behaviour and Mental Health 11:S77-S89, 2001Google Scholar
38. Mossman D: Evaluating violence risk "by the book": a review of HCR-20: Assessing Risk for Violence, version 2, and The Manual for the Sexual Violence Risk—20. Behavioral Sciences and the Law 18:781–789, 2000Crossref, Google Scholar
39. Witt PH: A practitioner's view of risk assessment: the HCR-20 and SVR-20. Behavioral Sciences and the Law 18:791–798, 2000Crossref, Google Scholar
40. Dempster RJ: Prediction of sexually violent recidivism: a comparison of risk assessment instruments. Burnaby, BC, Canada, Simon Fraser University, department of psychology, 1998 (unpublished master's thesis)Google Scholar
41. Webster CD, Eaves D, Douglas KS, et al: The HCR-20 Scheme: The Assessment of Dangerousness and Risk. Burnaby, BC, Canada, Mental Health, Law, and Policy Institute and Forensic Psychiatric Services Commission of British Columbia, 1995Google Scholar
42. Ross DJ, Hart SD, Eaves D, et al: The relationship between the HCR-20 and community violence in a sample of NCRMD outpatients. Presented at the Founding Conference of the International Association of Forensic Mental Health Services, Vancouver, BC, April 19 to 21, 2001Google Scholar
43. Douglas KS, Klassen C, Ross D, et al: Psychometric properties of HCR-20 violence risk assessment scheme in insanity acquittees. Poster presented at the annual meeting of the American Psychological Association, San Francisco, August 14 to 18, 1998Google Scholar
44. Ross DJ, Hart SD, Eaves D, et al: The relationship between the HCR-20 and BC Review Board decisions on the release of forensic psychiatric inpatients. Presented at the International Conference on Risk Assessment and Risk Management, Vancouver, BC, November 17 to 19, 1999Google Scholar
45. McNiel DE, Binder RL: The relationship between acute psychiatric symptoms, diagnosis, and short-term risk of violence. Hospital and Community Psychiatry 45:133–137, 1994Abstract, Google Scholar
46. McNiel DE, Binder RL: Screening for risk of inpatient violence: validation of an actuarial tool. Law and Human Behavior 18:579–586, 1994Crossref, Google Scholar
47. McNiel DE, Binder RL: Correlates of accuracy in the assessment of psychiatric inpatients' risk of violence. American Journal of Psychiatry 152:901–906, 1995Link, Google Scholar
48. Bartko JJ, Carpenter WT: On the methods and theory of reliability. Journal of Nervous and Mental Disease 163:307–317, 1976Crossref, Medline, Google Scholar
49. Cicchetti DV, Sparrow SA: Developing criteria for establishing interrater reliability of specific items: applications to assessment of adaptive behavior. American Journal of Mental Deficiency 86:127–137, 1981Medline, Google Scholar
50. Landis J, Koch GG: The measurement of observer agreement for categorical data. Biometrics 33:159–174, 1977Crossref, Medline, Google Scholar
51. Mossman D, Somoza E: ROC curves, test accuracy, and the description of diagnostic tests. Journal of Neuropsychiatry and Clinical Neurosciences 3:330–333, 1991Crossref, Medline, Google Scholar
52. Luke DA, Homan SM: Time and change: using survival analysis in clinical assessment and treatment evaluation. Psychological Assessment 10:360–378, 1998Crossref, Google Scholar
53. SPSS, version 10.1.0, Chicago, SPSS Inc, 2000Google Scholar
54. Hare RD: Manual for the Hare Psychopathy Checklist—Revised. Toronto, Multi-Health Systems, 1991Google Scholar
55. Dunlap WP: A program to compute McGraw and Wong's common language effect size indicator. Behavior Research Methods, Instruments, and Computers 31:706–709, 1999Crossref, Medline, Google Scholar
56. Cohen J: Statistical Power Analysis for the Behavioral Sciences, 2nd ed. Hillsdale, NJ, Lawrence Erlbaum, 1988Google Scholar
57. Dawes RM: The robust beauty of improper linear models in decision making. American Psychologist 34:571–582, 1979Crossref, Google Scholar
58. Dawes RM, Corrigan B: Linear models in decision making. Psychological Bulletin 81:95–106, 1974Crossref, Google Scholar
59. Dawes RM, Faust D, Meehl PE: Clinical versus actuarial judgment. Science 243:1668–1674, 1989Crossref, Medline, Google Scholar
60. Heilbrun K: Prediction versus management models relevant to risk assessment: the importance of legal decision-making context. Law and Human Behavior 21:347–359, 1997Crossref, Medline, Google Scholar
61. Douglas KS, Webster CD, Hart SD, et al (eds): HCR-20 Violence Risk Management Companion Guide. Burnaby, BC, Simon Fraser University, Mental Health Law and Policy Institute, and Tampa, Fla, University of South Florida, Department of Mental Health Law and Policy, 2001Google Scholar