Effects of Psychoeducation for Korean Americans With Chronic Mental Illness
Abstract
OBJECTIVE: Korean Americans' access to mental health services may be limited because of differences in their views of mental illness compared with Westerners, unfamiliarity with treatment methods, and cultural associations of social stigma with mental problems. This study used data from an urban outpatient clinic to assess the effects of a ten-week psychoeducational intervention for Korean Americans with chronic mental illness. METHODS: Forty-eight Korean-American adults with a diagnosis of schizophrenia were randomly assigned to either an experimental group that provided a culturally sensitive psychoeducational group program in addition to individual supportive therapy or a control group that offered only individual supportive therapy. The two groups were compared on pre- and posttreatment measures of psychiatric symptoms, attitudes about and understanding of mental illness, and coping skills. The experimental psychoeducational treatment group was expected to show lower symptom severity, greater understanding of mental illness leading to a decreased perception of stigma, and greater coping skills after the intervention than the control group. Comparisons were made with repeated-measures analysis of covariance with the effects of gender and education controlled for. RESULTS: Compared with the control group, the psychoeducational group showed significantly reduced symptom severity and perception of stigma and greater coping skills immediately after treatment. CONCLUSIONS: These findings suggest that a culturally sensitive psychoeducational intervention is a useful short-term treatment modality for Korean Americans with a diagnosis of schizophrenia.
Over the past few decades the number of Asian immigrants in the United States has increased substantially, and Koreans represent one of the fastest growing ethnic groups in the U.S. Asian population. At the time of the 1990 census, more than 350,000 Koreans lived in the United States (1), and by 2000 the number approached 1.1 million (2).
The prevalence of mental illness among Korean Americans is poorly documented. Available data, derived mainly from treatment sources, suggest that Korean Americans have had comparatively lower admission rates to mental health facilities and less use of mental health services than other ethnic groups (3). This low level of service use may be accounted for by lack of knowledge of existing resources and unfamiliarity with treatment methods as well as by the failure of mental health services to provide culturally relevant interventions (4,5).
Many Asian cultures, including Korean culture, do not have the same concrete definition of mental illness as the one used in mainstream American culture. For example, they do not distinguish psychological symptoms from physical ones and tend to regard both kinds of symptoms as signs of physiological disharmony and sickness (6). In addition, mental illness is associated with tremendous stigma. The concept of counseling or sharing one's problems outside the family is foreign to Koreans. As a result, many Korean Americans delay seeking help until a situation has reached a crisis state (7). The scarcity of bilingual services complicates access to care (8).
For Koreans with chronic mental illness, especially those who are recent immigrants, difficulties in adjusting to a new society are compounded by their illness and their reluctance to seek treatment. However, Korean patients do benefit from services in a continuing treatment program when staff members speak Korean and program activities include culturally relevant components (8). Nevertheless, many program clients cannot articulate their reasons for being in such programs and do not have a good understanding of the treatment modalities used in their care (9).
During the past 20 years, a variety of psychoeducational models have been developed and tested to address the needs of people with schizophrenia and their families. The impact of deinstitutionalization has also led to recognition of the need for more effective community management services and strategies (10). Advocacy for consumers' rights likewise has increased the use of psychoeducation to provide information to persons with chronic mental illness about their illness and treatment (11).
Hayes and Gantt (12) modified the family psychoeducational model for use with persons with chronic mental illness and demonstrated the positive effect that knowledge can have on participants' functioning and attitudes. They argued that psychoeducation decreases impairment by providing some sense of mastery, which in turn provides hope about the opportunity for a productive life. Learning about one's disease demystifies the illness and diminishes associated stigma.
Barter and colleagues (13) described the use of a psychoeducational approach for persons with chronic psychiatric illness in a community social rehabilitation program. They found that about 71 percent of the clients who received medical education showed an increased knowledge of antipsychotic medications. The day hospital program developed by Jeffries (11) focused on intensive education about schizophrenia. He observed that providing education about the illness enhanced self-esteem and increased the likelihood of treatment compliance.
Although a considerable body of literature addresses interventions for persons with severe mental illness and their families aimed at preventing relapses, facilitating rehabilitation, and promoting community mental health, many mental health professionals have not incorporated psychoeducation into their clinical work, and interventions have not been well adapted for culturally diverse populations (14,15). Yet current best practices suggest that some form of education for the person with the illness and for the family is a critical component of effective treatment (16,17).
The literature suggested that a psychoeducational program that stresses a biopsychosocial model for mental illness would be well accepted by Korean Americans, who generally place less focus on the affective realm (18). Korean Americans revere teaching and learning, so the use of educational methods can underscore the importance of the program for clients. Moreover, Korean clients are likely to feel more comfortable with a didactic format than with an interactive situation, because the former is less conducive to experiential types of sharing that require self-disclosure. Their culturally determined respect for experts and authority may help facilitate both the educational process and the therapeutic alliance. This study was implemented to test a brief psychoeducational intervention designed spe-cifically to address the needs of Korean Americans with a diagnosis of schizophrenia in a large city outpatient clinic.
Methods
Participants
Participants were recruited from a pool of 110 Korean patients with chronic mental illness who were receiving services at an outpatient mental health clinic in the borough of Queens in New York City. Because of the admission criteria for the continuing day treatment program, some of the participants may have had functional deficits, but all were ambulatory and able to travel to and from the program independently.
Any patient with a diagnosis of schizophrenia, schizoaffective disorder, or schizophreniform disorder was eligible for the study. Diagnoses were made by a Korean psychiatrist in accordance with DSM-IV criteria (19). Among 65 Korean patients who met diagnostic criteria, 48 consented to participate in the study. The groups were conducted between January and March 2000.
Procedures
Twenty-four patients were randomly assigned to the experimental group and 24 to the control group. The experimental treatment included ten weekly psychoeducational group sessions as well as weekly individual supportive sessions. Each of three psychoeducational groups included eight participants. The psychoeducational sessions were 90 minutes long. Members of the control group received only the ten individual supportive sessions, which were about 45 minutes long.
The psychoeducational sessions were conducted by the first author, who is a Korean-speaking psychiatric social worker. The weekly supportive sessions for patients in both groups were conducted by a second-year student in a master's degree program, who was supervised by the first author. All sessions were conducted in Korean. Each psychoeducational session included a variety of educational techniques designed to enhance the participants' learning and to maintain their attention. The first part of each session was conducted in lecture form and was followed by a question-and-answer and discussion period. As suggested by the work of Anderson, McFarlane, and others (20,21,22,23,24), the curriculum manual included modules on definitions of illness, medications and side effects, relapse prevention, crisis and illness management, stigma, communication and stress management skills, self-help, and community resources. Goals, objectives, and content were specified for each module to promote consistency of presentation across the three groups.
In addition, discussion of traditional disease concepts was integrated into the sessions. For example, Korean perspectives on shamanism, ailments, distress, diseases, fortune and misfortune, and life and death were discussed in the context of psychiatric illness. Psyche and soma were presented as two complementary aspects of life to encourage participants to understand how emotional functioning is related to physiological functioning. Visual aids, including charts and handouts, were used to reinforce the didactic materials. All written materials were provided in both Korean and English, and the oral presentations were in Korean. Particularly in the earlier sessions, the clinician played an active role in facilitating the group discussion to encourage and support exchange and sharing. Refreshments were served at every session to encourage attendance. To reinforce the interventions, parallel sessions, also conducted in Korean, were offered to family members of all participants. Before the first session, the 48 participants were provided with a brief description of the study and were asked to sign an informed consent form, following an approved institutional review board protocol.
Measures
Measures included a demographic information form, the Brief Psychiatric Rating Scale (BPRS) (25,26), the Stigma-Devaluation Scale (27), and the Family Crisis Oriented Personal Evaluation Scales (28). The BPRS was completed before and after the intervention in Korean by a bilingual Korean psychiatrist, who was blinded to participants' treatment modality. To maximize understanding and full response, the other scales were verbally presented to the study participants by the first author in Korean, and self-report answers were written down by the participants. Follow-up data were collected during the week after participants completed the ten-week program.
Demographic characteristics. A questionnaire was used to collect data on participants' age, sex, education, marital status, employment status, household composition, primary source of emotional support, length of illness, and history of hospitalization.
Psychiatric symptoms. The BPRS was used to measure the severity of psychiatric symptoms. The BPRS is a widely used instrument consisting of 24 items that measure anxiety, depression, thought disturbance, activation, hostility, hallucinations, and suspiciousness, as well as bizarre behavior, self-neglect, and suicidality (25,26). It was originally designed for use by clinical observers of inpatient psychiatric populations in psychopharmacological outcome studies. The items are rated on a scale from 1 to 7, with higher scores indicating increasing severity. For this study, the following three scores were used: mean total BPRS score; mean score for the positive symptoms of conceptual disorganization, suspiciousness, hallucinatory behavior, and unusual thought content; and mean score for the negative symptoms of emotional withdrawal, motor retardation, blunted affect, and disorientation.
Stigma. Stigma was measured with Link's Stigma-Devaluation Scale (alpha=.88) (27). The scale consists of 12 items that assess the extent to which respondents believe that most people devalue or discriminate against a person with a history of psychiatric treatment. The scale focuses on perceptions of stigma rather than stigmatizing experiences to encourage candid reporting. It has shown adequate internal consistency overall (alpha=.76).
Coping skills. The participant's perception of functioning and coping in relation to the family was assessed with the Family Crisis Oriented Personal Evaluation Scales (28). This instrument identifies problem-solving and behavioral strategies used by families in difficult situations. It was used in this study because of the importance of family in Korean society and because all participants either lived with or were in close daily contact with family. The instrument includes 30 items focusing on the person in relation to the family system (how individual family members handle internal difficulties and problems among themselves) and on the family in relation to the social environment (the ways in which the family externally handles problems or demands). The measure has excellent internal consistency and test-retest stability. Subscales measuring the following five aspects of coping were used in this study: social support; reframing, or redefining stressful events to make them more manageable; spiritual support; mobilizing family to acquire and accept help; and passive appraisal, or the ability to accept problematic issues.
Translation. The instruments were initially translated by the first author and subsequently reviewed by two Korean-American psychiatrists who are both bilingual and bicultural. The Korean versions of instruments were then translated back to English by a second bilingual and bicultural social worker. The retranslated versions were compared with the original English version, and ambiguities were corrected.
Results
Demographic characteristics
Table 1 summarizes the characteristics of the participants in the experimental and control groups. The mean age of the patients in the experimental groups was 39.5 years and of those in the control group, 34.7 years; the difference was not significant. The mean number of hospitalizations and the duration of residency in the United States for the two groups were comparable. The majority of participants in both groups resided with their family. Among those who lived away from their family, all reported daily contact with parents. Most participants had no children (70.8 percent of both the experimental and control groups), and the majority were either never married or divorced. Most participants in both groups were unemployed. All participants were taking one or more psychotropic medications and were described by their primary psychiatrist as compliant with treatment. No one in either group was hospitalized during the study period. No significant differences between the experimental and control groups were found for any sociodemographic variables. However, because a higher proportion of the participants in the psychoeducational group were female and had at least some college education, we controlled for gender and education by using analysis of covariance (ANCOVA).
Hypothesis testing
Three hypotheses were tested to assess the effect of psychoeducation on symptoms, experienced stigma, and coping skills in relations to the family at short-term follow-up during the week after the intervention. Hypothesis 1 proposed that the psychoeducational treatment group would show less severe symptoms, as measured by the total score on the BPRS and the BPRS subscales for positive and negative symptoms, than the control group. Hypothesis 2 was that participants in the psychoeducational treatment group would describe experiencing less stigma associated with mental illness, as measured by the Stigma-Devaluation Scale, than the control group. Hypothesis 3 proposed that, compared with the control group, participants in the psychoeducational treatment group would improve their perceived effectiveness in coping with family-related problems, as measured with subscales of the Family Crisis Oriented Personal Evaluation Scales.
Psychiatric symptoms. As Table 2 shows, the results of an ANCOVA controlling for gender and education showed that, for the sample as a whole, severity of symptoms as measured by the BPRS decreased over the course of treatment. The analysis of the interaction between time and treatment was also significant, demonstrating that, compared with the control group, the experimental group showed a significantly greater decrease in symptom severity over time.
To further examine the effect of psychoeducation on symptoms, ANCOVAs were conducted with data from the positive and negative subscales of the BPRS (Table 2). The sample as a whole showed a significant decrease in positive symptoms over time. Compared with the control patients, the experimental patients showed a significantly greater decrease in positive symptoms over time.No significant change in negative symptoms over time was found for all participants, and no significant difference in change over time between the experimental and control groups was found.
Stigma. As Table 3 shows, for the sample as a whole, there was a significant difference in the level of stigma and devaluation related to mental illness before and after the intervention. In addition, over the course of the treatment, the members of the experimental group assigned less stigma to mental illness than the control group.
Coping skills. As Table 3 shows, no significant difference over time in coping skills was found for the sample as a whole. However, coping skills for the experimental group improved significantly more than for the control group over the course of treatment. Findings for the subscales measuring social support, mobilizing the family, and reframing mirrored the findings for the full scale—scores did not increase over time for the sample as a whole, but the experimental group improved significantly more than the control group from pretreatment to posttreatment. The two remaining scales followed a somewhat different pattern. On the subscale measuring passive appraisal, all participants improved significantly over time, and the experimental group improved significantly more than the control group from pretreatment to posttreatment. However, for the subscale measuring spiritual support, there was no change either over time or related to treatment.
Discussion and conclusions
Both the experimental group and the control group responded well to the intense treatment provided. Of critical importance is the finding that the psychoeducational program was associated with a reduction in both total and psychotic (positive) symptoms among the experimental patients. It appears that the participants were able to use the skills gained through this program to manage some of their symptoms, at least immediately after treatment.
The experimental group expressed significantly less perceived stigma associated with mental illness after treatment than the control group. This finding suggests that a greater understanding and knowledge of mental illness can modify clients' perceptions of the stigma attached to psychiatric disorders. To change attitudes, it may be important for the client to be consistently exposed to new information that can be integrated into his or her outlook.
The predicted positive influence of psychoeducation on increasing coping skills was partly supported. Findings for the Family Crisis Oriented Personal Evaluation Scales showed that scores for passive appraisal increased for all participants, and participants in the psychoeducational groups did better over time. Not surprisingly, those in the psychoeducational groups also improved significantly over time on subscales measuring social supports and ability to reframe situations and mobilize the family. These findings imply that Korean immigrants can be motivated to turn to relatives, friends, and acquaintances for help with emotional, psychological, and relational problems. In turn, relationships with these sources of help can be developed by the clinician as useful adjuncts to successful treatment.
Implications for clinical practice
The findings support the idea that educating persons with chronic mental illness by using culturally sensitive psychoeducational techniques is a valuable component in a comprehensive approach to the treatment of schizophrenia. From a clinical perspective, psychoeducation appeared to enhance the participants' knowledge of Western concepts of mental illness and treatment, at least at short-term follow-up during the week after the intervention. Bridging Eastern and Western views of mental illness and treatment also seemed to increase the likelihood that the Korean clients would use and accept mental health services in the United States.
The positive results suggest that the psychoeducational program, as a culturally sensitive intervention, is useful for facilitating the adaptation of Korean-American clients to mental health services in the United States and for generating knowledge that could be helpful in the delivery of services to ethnic minority groups. In this psychoeducational approach, the clinician acts in the role of culture broker, interpreting cultural differences and providing linkage between the ethnic group and the services available in the mainstream society. Through such work, a member of a minority group can be encouraged to draw on new experiences and knowledge to suit his or her particular circumstances.
Psychoeducation provides a cognitive framework that helps people understand their illness and the rationale for treatment. This framework may assist them in accepting their illness and increasing treatment compliance as the result of enhanced awareness and familiarity with treatment techniques. Such an approach may help correct myths and prejudices toward mental illness by providing information in a context of cultural relevance, safety, respect, and hope and by extending the intervention to family members as well.
Implications for future research
A major strength of this study was its attempt to explore the culturally specific psychoeducational needs of Korean-American patients with severe mental illness and to help consumers bridge the gap between Korean and Western perceptions of mental illness. It is among the first studies of Korean Americans to consider Korean cultural values as an important influence to be aware of when providing psychoeducation. By investigating the interrelationship between culture and mental health, the study may help mental health professionals design treatment that transcends cultural and linguistic barriers.
Despite these strengths, the study had certain limitations. First, the study was limited to a relatively small sample of Korean-American persons living in New York City. This group does not present a complete picture of Korean newcomers and cannot be generalized to Korean immigrants elsewhere in the United States. Second, the experimental intervention was conducted by a Korean-speaking clinician who also collected most of the data for the analyses, introducing the potential for bias. Finally, the study examined only the short-term effects of the intervention. The long-term effects remain unknown. Although the experimental participants appear to have had gains in certain areas, it is possible that the gains will not be sustained.
A longitudinal study is needed to see how Korean Americans with chronic mental illness respond to psychoeducation over time. Studies using larger samples and designed to measure the long-term as well as the short-term effects would generate additional valuable information about the effectiveness of this treatment intervention.
Qualitative methods might also be used to further explore some of the questions raised by this study, in an effort to more fully understand cultural barriers and the treatment needs of Korean Americans with severe mental illness. Comparative studies involving various racial and ethnic minority groups in this country would shed light on these needs as well. Community-based studies could provide the information needed to design programs to lessen the stigma associated with mental illness and to create a more accepting social and treatment environment for Korean Americans with mental illness. Such programs could enhance Korean-American patients' understanding of mental health and mental illness and of the benefits of early treatment and community support.
Dr. Shin is assistant professor in the department of social welfare at the Graduate School of Theology of Sogang University in Seoul, Korea. Dr. Lukens is associate professor at the Columbia University School of Social Work and research scientist at the New York State Psychiatric Institute. Address correspondence to Dr. Lukens at Columbia University School of Social Work, 622 West 113th Street, New York, New York 10025 (e-mail, [email protected]).
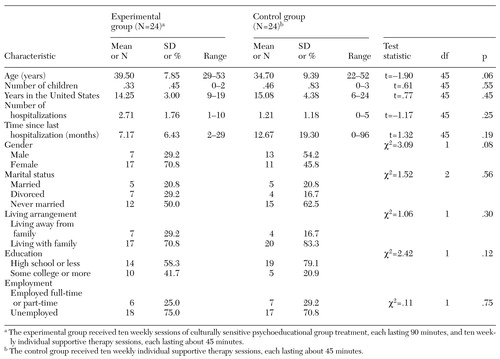 |
Table 1. Characteristics of Korean-American patients with schizophrenia in a study of a culturally sensitive psychoeducational group treatment program
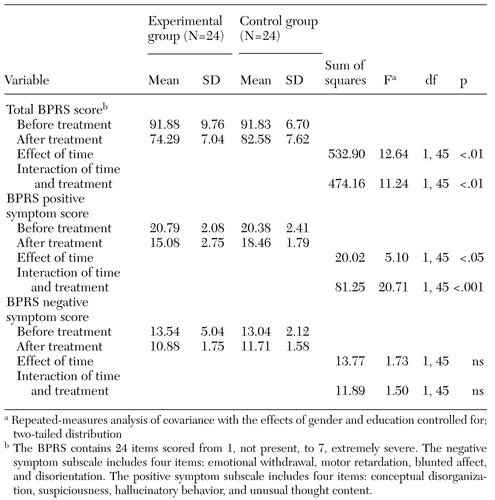 |
Table 2. Scores on the Brief Psychiatric Rating Scale (BPRS) of Korean-American patients with schizophrenia before and after treatment in a study of a culturally sensitive psychoeducational group treatment program
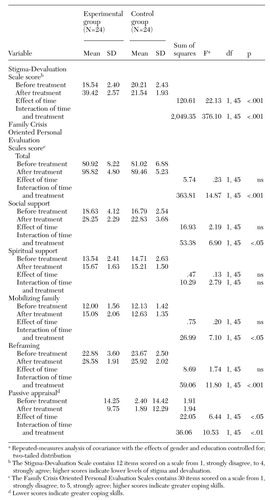 |
Table 3. Scores on the Stigma-Devaluation Scale and the Family Crisis Oriented Personal Evaluation Scales of Korean-American patients with schizophrenia before and after treatment in a study of a culturally sensitive psychoeducational group treatment program
1. 1990 Census of the Population: General Population Characteristics. Washington DC, US Bureau of the Census, 1990Google Scholar
2. 2000 Census of the Population: General Population Characteristics. Washington, DC, US Bureau of the Census, 2000Google Scholar
3. Ibrahim F: Effectiveness in cross-cultural counseling and psychotherapy: a framework. Psychotherapy 22:321-323, 1985Crossref, Google Scholar
4. Chin J: Diagnostic considerations in working with Asian Americans. American Journal of Orthopsychiatry 53:100-109, 1983Crossref, Medline, Google Scholar
5. Lorenzo M, Adler D: Mental health services for Koreans in a community health center. Social Casework 65:600-614, 1984Crossref, Medline, Google Scholar
6. Kim L: Psychiatric care of Korean Americans, in Culture, Ethnicity, and Mental Illness. Edited by Gaw AC. Washington, DC, American Psychiatric Press, 1993Google Scholar
7. Kwon-Ahn Y: The Korean Protestant Church: The Role in Service Delivery for Korean Immigrants. Doctoral dissertation. New York, Columbia University, School of Social Work, 1987Google Scholar
8. Shin J: Help-seeking behaviors by Korean immigrants for their depression. Doctoral dissertation. New York, Columbia University, School of Nursing, 1999Google Scholar
9. Chun C, Sue S: Mental health issues concerning Asian Pacific American children, in Struggling to Be Heard: Unmet Needs of Asian Pacific American Children. Edited by Pang VO, Cheng LL. Albany, State University of New York Press, 1998Google Scholar
10. McGill C, Falloon I, Boyd J, et al: Family educational intervention in the treatment of schizophrenia. Hospital and Community Psychiatry 34:934-938, 1983Abstract, Google Scholar
11. Jeffries J: Educative approaches in therapy, in New Perspectives in Schizophrenia. Edited by Menuck M, Seeman M. New York, Macmillan, 1985Google Scholar
12. Hayes R, Gantt A: Patient psychoeducation: the therapeutic use of knowledge for the mentally ill. Social Work in Health Care 17:53-67, 1992Crossref, Medline, Google Scholar
13. Barter J, Queirolo J, Ekstrom S: A psychoeducational approach to educate chronic mental patients for community living. Hospital and Community Psychiatry 35:793-797, 1984Abstract, Google Scholar
14. Lam D: Psychosocial family intervention in schizophrenia: a review of empirical studies. Psychological Medicine 21:423-441, 1991Crossref, Medline, Google Scholar
15. Lukens EP, Thorning H, Herman DB: Family psychoeducation in schizophrenia: emerging themes and challenges. Journal of Practical Psychiatry and Behavioral Health 5:314-325, 1999Crossref, Google Scholar
16. American Psychiatric Association: Practice Guideline for the Treatment of Patients With Schizophrenia. American Journal of Psychiatry 154(4 suppl):1-63, 1997Google Scholar
17. McEvoy J, Scheifler P, Frances A: Expert Consensus Guidelines Series: Treatment of Schizophrenia, 1999. Journal of Clinical Psychiatry 60(suppl 11):3-80, 1999Medline, Google Scholar
18. Hurh W, Kim K: Correlates of Korean immigrants' mental health. Journal of Nervous and Mental Disease 178:703-711, 1990Crossref, Medline, Google Scholar
19. Diagnostic and Statistical Manual of Mental Disorders, 4th Edition. Washington, DC, American Psychiatric Association, 1994Google Scholar
20. Anderson C, Reiss D, Hogarty G: Schizophrenia and the Family: A Practitioner's Guide to Psychoeducation and Management. New York, Guilford Press, 1986Google Scholar
21. McFarlane W, Lukens E, Link B, et al: Multiple family groups and psychoeducation in the treatment of schizophrenia. Archives of General Psychiatry 52:679-687, 1995Crossref, Medline, Google Scholar
22. Bernheim K, Lehman A: Working with Families of the Mentally Ill. New York, Norton, 1985Google Scholar
23. Lukens E, Thorning H: Psychoeducation and severe mental illness: implications for social work practice and research, in Breakthroughs in Mental Health Research: Implications for Social Work Practice. Edited by Williams J, Ell K. Washington, DC, NASW Press, 1998Google Scholar
24. Falloon I, Boyd J, McGill C: Family Care of Schizophrenia. New York, Guilford Press, 1984Google Scholar
25. Overall J, Gorham D: The Brief Psychiatric Rating Scale. Psychological Report 10:799-812, 1962Crossref, Google Scholar
26. Guy W (ed): ECDEU Assessment Mental for Psychopharmacology. Pub No (ADM) 76-338. Washington, DC, US Department of Health, Education, and Welfare, 1976Google Scholar
27. Link B: Understanding labeling effects in the area of mental disorders: an assessment of the effects of expectations of rejection. American Sociological Review 52:96-112, 1987Crossref, Google Scholar
28. McCubbin H, Thompson A, McCubbin M: Family Assessment: Resiliency, Coping, and Adaptation. Madison, University of Wisconsin Press, 1996Google Scholar