Datapoints: Medicaid Managed Care and Substance Abuse Treatment
Conversion of Medicaid substance abuse treatment to managed care has raised concerns about access. However, several states have expanded Medicaid eligibility criteria at the same time. Proponents argue that increasing Medicaid enrollment will ease access to treatment for previously uninsured individuals. It is also possible, however, that Medicaid expansion represents cost shifting from state to federal payers. If so, there would likely be no net increase in publicly funded substance abuse treatment admissions after Medicaid expansion.
Another concern is "cream skimming" —giving treatment preferentially to clients whose illness is less severe. Thus the average severity of illness of those treated would decrease after conversion to managed care.
Data to test these hypotheses were obtained from a Medicaid demonstration project in Oregon. Data elements from the Oregon Client Process Monitoring System were combined to generate a severity index. In a prospective study, the severity measure was found to be highly correlated with clinicians' ratings of clients according to the placement criteria of the American Society of Addiction Medicine and with Addiction Severity Index ratings obtained via client interviews.
Figure 1 plots the number of adult clients admitted for the three years before substance abuse treatment was integrated into Medicaid managed care in 1995 and the five years afterward. Medicaid admissions started to increase before the integration of substance abuse treatment because eligibility was expanded in 1994 under a federal Section 1115 waiver. After a modest initial reduction in the number of uninsured clients, the total number of publicly funded clients increased dramatically, primarily as a result of expanded Medicaid eligibility.
Figure 2 plots the average severity index for clients admitted during the same period for treatment services covered or not covered by Medicaid. Little change in severity was observed for the Medicaid clients entering outpatient or methadone maintenance treatment, and little deviation was noted from the pattern observed for residential and detoxification services not covered by Medicaid.
In a previous study (1) we found that access rates increased for clients eligible for Medicaid in Oregon after the shift to managed care. In the study reported here we found little evidence that cost shifting or skimming contributed to this increased access.
Acknowledgments
This research was supported in part by grant R01-DA-11970 from the National Institute on Drug Abuse and by cooperative agreement 1UR-7TI-1129401 and grant 1KD-1TI-12045-01 from the Substance Abuse and Mental Health Services Administration.
Dr. Deck is senior research associate at RMC Research Corporation, 522 S.W. Fifth Avenue, Suite 1407, Portland, Oregon 97204 (e-mail, [email protected]). Dr. McFarland is with the department of psychiatry at the Oregon Health Sciences University in Portland. Harold A. Pincus, M.D., and Terri L. Tanielian, M.A., are editors of this column.
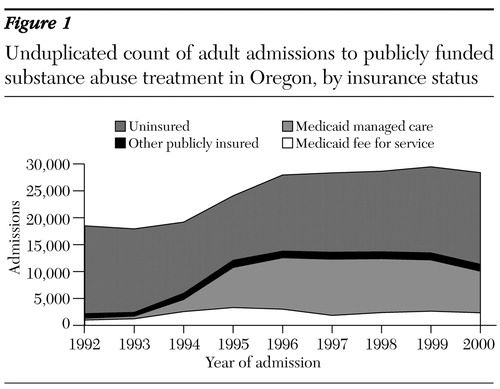
Figure 1. Unduplicated count of adult admissions to publicly funded substance abuse treatment in Oregon, by insurance status
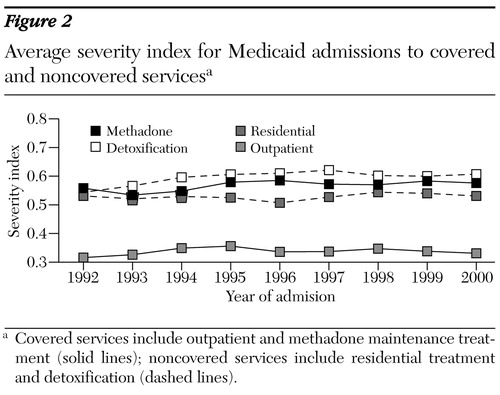
Figure 2. Average severity index for Medicaid admissions to covered and noncovered servicesa
a Covered services include outpatient and methadone maintenance treatment (solid lines); noncovered services include residential treatment and detoxification (dashed lines).
. Deck DD, McFarland BH, Titus JM, et al: Access to substance abuse treatment under the Oregon Health Plan. JAMA 284:2093-2099, 2000Crossref, Medline, Google Scholar



