Psychopharmacology: Use of Psychotropics in Two Employee Groups Directly Affected by the Events of September 11
The terrorist attacks of September 11, 2001, perhaps more than any preceding event, most immediately and directly affected the employed population. By September 12, employers rushed to provide mental health care to their employees. Emergency help was provided to current employees and their dependents and was even made available to the general public free of charge (1). Since September 11, early anecdotes of increased need for mental health care have been supported by empirical observations. Schuster and colleagues (2) reported that 90 percent of the 560 people they surveyed had at least one symptom of stress associated with the incident. New prescriptions for antianxiety drugs had increased by 25 percent nationwide in October 2001 (3). The events of September 11 clearly had immediate and dramatic effects on the mental health needs of individuals, and these immediate needs were often met with a short-term increase in a specific form of mental health emergency services—critical incident stress debriefings, provided mostly by managed behavioral health organizations (1).
Despite these immediate responses, recent reports suggest that many signs of distress persist (4). Although there is evidence of enduring distress and dysfunction, an increase in the use of mental health specialty services is not readily apparent (1). Perhaps people who need longer-term follow-up care, even those who are employed, are not seeking appropriate services. For example, Rosenheck (5) found no substantial change in the use of outpatient services after September 11 among patients in Department of Veterans Affairs facilities in New York and concluded that the event was not as medically significant as had been anticipated.
This study, from one managed behavioral health organization—United Behavioral Health (UBH)—examined the use of psychopharmaceuticals over the longer term in two employed populations. To the extent that an employed population would be expected to have fewer barriers to care than an unemployed population, we expected that the use of psychopharmaceuticals would increase with need. We focused on the use of pharmaceuticals because previous studies showed a short-term increase in their use after September 11 (3) and because of the substantial role of pharmaceuticals in the treatment of the most common expected problems—anxiety and mood disorders.
To study the longer-term effects on the employed population, we compared forecasted drug use with actual drug use in two large, national employer groups. Both were directly and immediately involved in the events of September 11, and both reported substantial direct losses. We measured the use of four classes of pharmaceuticals before and after September 11: any pharmaceutical medication, any psychotropic medication, antidepressant medications only, and antianxiety medications only. We also obtained data on the specialization of the prescribing physicians—for example, psychiatrist versus nonpsychiatrist.
Methods
We measured the use of pharmaceuticals for two years before and five months after September 11, 2001. We conducted time-series analyses to determine the expected or forecasted use of pharmaceuticals after September 11. Forecasted use was then compared with actual use. We used monthly administrative data on pharmaceutical claims maintained by United Health Group (UHG) and extracted for each employer group. (UBH is a wholly owned subsidiary of UHG.)
The two employer groups were chosen because, as a function of their industries and geography, both were highly involved in the events of September 11 and both were high users of critical incident stress debriefings immediately after the disaster. The number of insured enrollees employed by employer 1 ranged from approximately 30,000 in 2000 to 150,000 in 2002. For employer 2, the number ranged from approximately 3,500 in 2000 to 3,000 in 2002. Both employer groups had broad managed mental health care benefit plans with UBH and pharmaceutical management benefits with UHG.
Specific drug categories were identified on the basis of pharmaceutical therapeutic class codes. The all-pharmaceuticals category included any type of pharmaceutical. The any-psychotropic category included only psychotropic medications that were identified by using the generic therapeutic class for psychotherapeutic drugs (code 80). The antidepressant category included only antidepressant medications that were selected by using the American Hospital Formulary Service (AHFS) classification code for antidepressants (code 281604). The antianxiety category included only antianxiety medications that were identified by using the AHFS classification code for anxiolytics, sedatives, hypnotics, and benzodiazepines (codes 2824, 282400, 282408, and 282492).
Individual users per month were calculated as a percentage of the total monthly membership eligible for the pharmaceutical benefit. We determined the total cost of pharmaceuticals and calculated the increase per member per month. The Drug Enforcement Administration registration number system, in combination with information about provider specialization, was used as an indication of whether the pharmaceuticals had been prescribed by a psychiatrist.
To test for statistically significant differences from previous years, seasonal decomposition and forecasting were applied by using an autoregressive integrated moving-average model with first-order differencing to address stationarity. A 95 percent confidence interval (standard error=1.96) around the forecasted time series was used to determine significance. Actual values that fell outside of the confidence interval were determined to be significantly different from the forecasted value at an alpha of .05 or less.
Results
All significant effects observed were in the antianxiety medication category. The use of antianxiety medications after September 11, 2001, is illustrated in Figures 1 and 2. Only slight increases in the other categories of pharmaceuticals—any pharmaceutical, any psychotropic, and antidepressants—were observed, and they were not significantly different from forecasted levels.
Both measures of increased use of antianxiety medications were significantly different from forecasts made in October 2001. In December, only per-member-per-month spending showed an increase. These effects were more than what would be expected on the basis of use in the previous two-year period and were seen most consistently in October 2001, when increased spending and the proportion of users was greater than in October of previous years after adjustment for the existing slower-wave trend in pharmaceutical spending.
An examination of prescribing physicians' specialties suggested that a majority of antianxiety medications (more than 85 percent) were prescribed by nonpsychiatrists. Although there was a slight increase in the proportion of nonpsychiatrists prescribing antianxiety medications during September and November 2001, this increase was not statistically significant given the variability observed in previous years.
Discussion and conclusions
An immediate increase in the use of antianxiety medications was to be expected after an event such as the terrorist attacks of September 11, 2001, in populations directly affected by the attacks. Perhaps most surprising was that the use of antidepressants and other psychotropic medications did not increase significantly. On the basis of previous reports (3), an increase in antidepressant use was expected, especially among those who experienced a loss as a result of the terrorist attacks. The pattern we found is even more surprising in light of the growing evidence of the comorbidity of anxiety and depression (greater than 40 percent) (6).
The lack of evidence of an increase in the use of antidepressants was in line with previous reports of no increases in mental health services provided at Department of Veterans Affairs facilities in New York, Washington, D.C., and several other large U.S. cities (5). Analyses of all available data on the use of specialty care at UBH, including employee assistance programs, did not show any significant increase in use after September 11 (1). In a recent survey of participants in mental health debriefings in New York City, only 2 percent of participants reported that they sought mental health services after participating in a psychoeducational debriefings (7). For some patients, the use of antianxiety medications to relieve symptoms may not require concomitant psychotherapeutic services; however, for many patients psychotherapy is essential. Furthermore, antidepressants may be more effective than antianxiety medications for patients with posttraumatic stress disorder (8). Although it is not surprising that large numbers of persons affected by the terrorist attacks contacted their physician for relief within weeks of September 11—and it is natural that some care would be manifested in antianxiety prescriptions from primary care physicians—it is surprising that the increase in prescriptions did not appear to be coupled with a significant increase in the use of specialty care services.
An immediate increase was noted in the use of critical incident stress debriefings in September (1) and antianxiety medications in October in the employed population. Yet persistent and longer-term needs (4) did not appear to lead to an increase in the use of specialty mental health services (1,7). Perhaps the lack of help-seeking behavior observed after September 11 is not unique to this event but is more perennial, occurring after most traumatic events—for example, the sudden death of a close family member or injury due to violence or an auto accident (9). To the extent that the events of September 11 were perceived by most people to have been of no greater severity than other personal traumatic events, many individuals may have engaged in established coping strategies that did not include seeking professional help. Also, we suggest that because of the universality of the experience, communal supportive responses may also have mitigated help-seeking behavior from mental health professionals. The influence of critical incident stress debriefings on the use of other care resources deserves examination.
Afterword by the column editor: After the terrorist attacks of September 11, 2001, it was predicted that the mental health resources available in New York could be overwhelmed providing treatment to tens of thousands of traumatized individuals. Yet McCarter and Goldman's finding of only a time-limited increase in prescriptions of anxiolytics by primary care providers is one of several reports that show no spike in the use of specialty mental health services after September 11 among providers serving populations with a high level of exposure to the attacks.
Several recent studies found elevated rates of trauma symptoms several months after September 11 among persons who were highly exposed to the terrorist attacks. Reactions of anxiety, grief, and depression are common after such a catastrophe, and for most people they are transient. Many individuals may choose to cope by seeking the help of family or friends or seeking relief of for the most troublesome symptoms, such as sleep disturbance, rather than seeking specialty mental health services. Others, however, may avoid mental health providers because of stigma, cost, or other barriers. Finally, compared with other disorders, such as depression, the public may not know about the effective treatments that have been developed for posttraumatic stress disorder (PTSD) and other anxiety disorders or may not know where to find providers who can deliver these treatments.
One recent study estimated that the rate of PTSD among New York City residents was 11 percent. Further research is needed to explain the lack of a corresponding spike in the use of specialty mental health services. Understanding how much is the result of lack of need and how much is the result of unmet need is an important step in understanding how to best meet the psychological needs of a population after a catastrophic event.
Acknowledgments
The authors thank Brian Cuffel, Ph.D., and Bradley D. Stein, M.D., M.P.H., for their helpful comments.
The authors are affiliated with the department of behavioral health sciences at United Behavioral Health, 425 Market Street, 27th Floor, San Francisco, California 94105 (e-mail, [email protected]). George M. Simpson, M.D., is editor of this column.
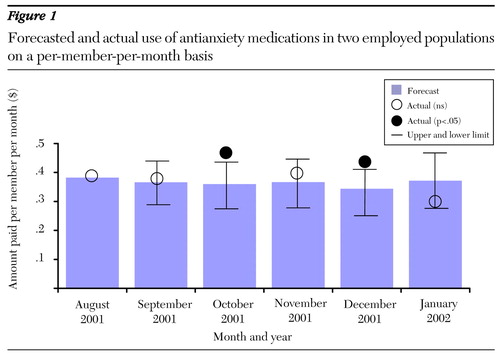
Figure 1. Forecasted and actual use of antianxiety medications in two employed populations on a per-member-per-month basis
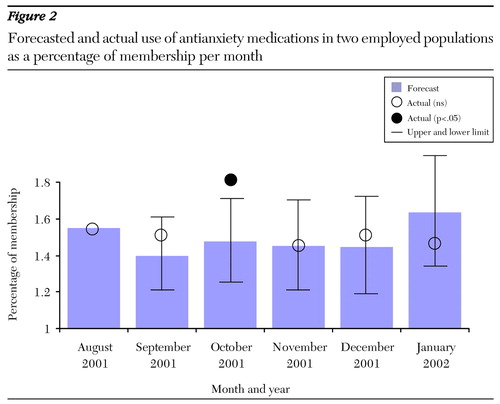
Figure 2. Forecasted and actual use of antianxiety medications in two employed populations as a percentage of membership per month
1. Goldman W: Terrorism and mental health: private-sector responses and issues for policy makers. Psychiatric Services 53:941-943, 2002Link, Google Scholar
2. Schuster MA, Stein BD, Jaycox L, et al: A national survey of stress reactions after the September 11, 2001, terrorist attacks. New England Journal of Medicine 345:1507-1512, 2001Crossref, Medline, Google Scholar
3. Agovino T: Use of anti-anxiety drugs surging. Associated Press, Oct 12, 2001Google Scholar
4. Goodnough A: Post-9/11 pain found to linger in young minds. New York Times, May 2, 2002. Available at http://www.nytimes.com/2002/05/02/health/02scho.htmlGoogle Scholar
5. Rosenheck R: Reactions to the events of September 11. New England Journal of Medicine 346:629, 2002Crossref, Medline, Google Scholar
6. De Graaf R, Bijl RV, Smit F, et al: Risk factors for 12-month comorbidity of mood, anxiety, and substance use disorders: findings from the Netherlands Mental Health Survey and Incidence Study. American Journal of Psychiatry 159:620-629, 2002Link, Google Scholar
7. Herman R, Kaplan M, LeMelle S: Psychoeducational debriefings after the September 11 disaster. Psychiatric Services 53:479, 2002Link, Google Scholar
8. Hageman I, Anderson H, Jorgensen M: Post-traumatic stress disorder: a review of psychobiology and pharmacotherapy. Acta Psychiatrica Scandinavica 104:411-422, 2001Crossref, Medline, Google Scholar
9. Zatzick DF, Kang SM, Muller HG, et al: Predicting posttraumatic distress in hospitalized trauma survivors with acute injuries. American Journal of Psychiatry 159:941-946, 2002Link, Google Scholar



