Insight Into Illness and Attitudes Toward Medications Among Inpatients With Schizophrenia
Abstract
This study assessed symptoms, severity of illness functional level, insight into illness, and attitudes toward medication in a sample of psychiatric patients who were newly admitted to a state hospital. The patients were evaluated before and after treatment with atypical, conventional, or mixed (atypical plus conventional) antipsychotic medication regimens with the Brief Psychiatric Rating Scale (BPRS), the Clinical Global Impression, the Global Assessment of Functioning, the Scale to Assess Unawareness of Mental Disorder, and the Drug Attitude Inventory. Overall, the patients showed significant improvement in symptoms, severity of illness, functional level, and insight into their illness during the course of hospitalization. Their attitudes toward medications changed minimally during treatment. Only the patients who were treated with conventional antipsychotics showed significant improvement in their attitudes toward medication. However, the change was not large enough to differentiate the conventional antipsychotic treatment group from the other treatment groups.
Among persons with schizophrenia, insight into illness and attitudes toward medications, along with the better recognized domains of symptoms, severity of illness, and functioning, are known to be important in determining outcomes (1,2,3). For some patients with schizophrenia, the use of atypical antipsychotics may be associated with reduced side effects, better compliance, and a lower rate of relapse (4). However, it is not entirely clear how the atypical antipsychotic medications affect insight into illness or attitudes toward medications relative to the older agents. It has been suggested that personal characteristics such as attitudes toward health and illness may be critical in determining attitudes toward medications (3). These factors may diminish the relative importance of medication-related side effects in treatment adherence. For example, Weiden and colleagues (5) reported that distress due to side effects was not necessarily associated with nonadherence among persons with schizophrenia who were followed up as outpatients.
In this study we prospectively assessed symptoms, severity of illness, functional level, insight into illness, and attitudes toward medications among patients with schizophrenia or schizoaffective disorder who were newly admitted to an acute care state psychiatric facility. We hypothesized that, independently of the type of antipyschotic medications used, symptoms, severity of illness, functional level, and insight into illness would all improve with treatment, whereas attitudes toward medication would probably not.
Methods
The study participants were patients who were newly admitted to either of two large acute care state psychiatric facilities. Patients who were eligible for the study had an admitting DSM-IV diagnosis of either schizophrenia or schizoaffective disorder. The participants were evaluated at admission and at discharge on measures of symptoms, severity of illness, functional level, insight into illness, and attitudes toward medications during the time they received usual treatment, which included medication treatment and unit-based psychosocial treatments for all patients. The study was completed between November 1999 and July 2000. Prior approval was obtained from the local institutional review board.
Patients were entered into the study within three days of admission to the hospital and were assessed with the Brief Psychiatric Rating Scale (BPRS) (6) to evaluate psychosis, the Clinical Global Impressions (CGI) scale (7) to evaluate general severity of illness, the Global Assessment of Functioning (GAF) (5) to evaluate their functional level, the Scale to Assess Unawareness of Mental Disorder (SUMD) (abbreviated version) (1) to evaluate their insight into their illness, and the Drug Attitude Inventory (DAI) (abbreviated version) (3) to evaluate their attitudes toward medications. The DAI (abbreviated version) is a relatively widely used ten-item self-report inventory that focuses on the subjective effects of antipsychotic medications among patients with schizophrenia. The SUMD (abbreviated version) is a well-validated nine-item scale that assesses awareness of illness among psychiatric patients, particularly those who have psychosis.
All rating scales were readministered within three days of discharge from the hospital after the treating clinician had determined that the patient had achieved clinical stability. Changes in scores on the rating scales were evaluated after antipsychotic medication treatment. The patients were classified into three groups: those who received atypical antipsychotic medications, those who received conventional antipsychotic medications, and those who were on a mixed (atypical plus conventional) antipsychotic regimen.
The data analysis used a baseline follow-up repeated-measures design. Differences between the three groups were tested by using one-way analysis of variance, and within-subjects effects measuring change from baseline to follow-up were tested by using difference t tests for the sample overall and by medication group. Post hoc between-subjects comparisons were conducted by using Tukey's honestly significant difference t test.
Results
Forty-five patients initially entered the study. The mean±SD age of the patients was 38.7±10.5 years. Thirty-one patients (69 percent) were men, and 14 (31 percent) were women. Thirty-three patients (73 percent) had schizophrenia, and 12 (27 percent) had schizoaffective disorder. Comorbid substance abuse was noted for ten patients (22 percent). Length of stay was about 12 days for all groups, except for the group of patients who were on a mixed antipsychotic regimen, whose mean length of stay was 22 days.
Nonadherence to an antipsychotic medication regimen before hospital admission—defined as not taking the prescribed medications at a frequency or dosage that would be expected to produce an antipsychotic effect—was a significant problem in this group of patients. Only eight patients (18 percent) had been adherent before admission, whereas 36 patients (80 percent) had not. Adherence could not be clearly determined for one patient.
Of the 45 patients who initially entered the study, 37 could be assessed at admission and at discharge. One patient did not receive a prescription for an antipsychotic medication at discharge. The study method did not allow us to establish the reason that this patient did not receive an antipsychotic medication. For the most part, the patients received the same medications in the hospital that they had been prescribed before admission. Thus 36 patients were included in the final analysis.
In general, the patients showed significant improvements in their psychotic symptoms, severity of illness, functional level, and insight into illness during the course of hospitalization. However, their subjective attitudes toward medications did not change significantly.
Of the 36 patients assessed who received prescriptions for antipsychotic medications, 20 (56 percent) received a prescription for an atypical antipsychotic medication at discharge, 11 (31 percent) received a prescription for a conventional antipsychotic, and five (14 percent) received a prescription for a combination of atypical and conventional antipsychotic medications. No significant differences between groups were observed in psychiatric diagnoses, duration of illness, comorbid psychiatric illness, race, or gender. However, the patients who received prescriptions for atypical antipsychotic medications were significantly younger on average than the patients in the other two groups. The three groups did not differ in terms of adherence to a prescribed medication regimen before admission.
Changes in symptoms, severity of illness, functional level, insight into illness, and attitudes toward medications between admission and discharge are summarized in Table 1. BPRS scores improved significantly in all three treatment groups. CGI, GAF, and SUMD scores improved only among patients who received atypical or conventional antipsychotics. DAI scores improved only among patients who received conventional antipsychotics. However, none of these changes were associated with significant between-subjects effects. Thus although the patients who received conventional antipsychotics demonstrated a statistically significant change in their attitudes toward medications during treatment, the change was not large enough to differentiate these patients from the other treatment groups.
Discussion and conclusions
This study was a naturalistic evaluation of psychiatric symptoms, severity of illness, insight into illness, and attitudes toward medications among patients with schizophrenia or schizoaffective disorder who were treated in an acute care state hospital setting. Limitations of the study include its use of a small sample, its short duration, its lack of a standardized diagnostic assessment instrument for assigning a primary diagnosis, and its nonblinded, nonrandomized design.
Overall, the patients in this study showed improvements in symptoms, severity of illness, and insight into their illness during their inpatient psychiatric treatment. Other investigators have similarly reported that both symptoms and insight significantly improved during hospital treatment among patients admitted to an acute care psychiatric unit (8,9). Weiler and colleagues (8) have suggested that some aspects of insight into illness are related to mental state during exacerbation of illness among patients with schizophrenia. We found no significant differences between our three groups of patients in previous adherence to prescribed medication regimens, symptoms, functional level, or insight into illness. It is possible that the small size of the sample prevented the detection of a significant difference between the treatment groups, and failure to detect significant differences between treatment groups does not necessarily mean that all treatments are equivalent.
Interestingly, the patients' attitudes toward medication changed minimally during treatment, and no significant differences were observed in attitudes toward medications between the three groups of patients who were treated with atypical antipsychotics, typical antipsychotics, or mixed medication regimens. Again, it is possible that our use of a small sample may have prevented the detection of significant differences.
Alternatively, in this state hospital population, medication-related adverse effects might not have been the driving component of attitudes toward medication. Additional factors that have been shown to contribute to negative attitudes toward medications for symptoms of schizophrenia include demographic characteristics, psychiatric characteristics, depressive state, and the patient's values and attitudes toward health and illness (3). It has been suggested that acceptance or acknowledgment of psychotic illness does not necessarily correspond to an acceptance of the risks and benefits of medication treatment for the illness (10). A better understanding of patients' perceptions of treatment and illness and their subjective experience is needed to more fully address the components of treatment and illness that are important to individuals with schizophrenia.
Acknowledgment
This study was supported in part by a grant from Janssen Research Foundation.
Dr. Sajatovic, Dr. Rosch, Dr. Sivec, and Dr. Sultana are affiliated with the department of psychiatry of Case Western Reserve University School of Medicine, University Hospitals of Cleveland, Hanna Pavilion, 11100 Euclid Avenue, Cleveland, Ohio 44106 (e-mail, [email protected]). Dr. Smith is with the Medical College of Ohio and with Northcoast Behavioral Healthare in Toledo. Dr. Alamir is with the Nord Center in Lorain, Ohio. Dr. Buckley is with the department of psychiatry of the Medical College of Georgia in Augusta. Dr. Bingham is with the Serious Mental Illness Treatment, Research, and Evaluation Center of the Veterans Health Administration and the University of Michigan in Ann Arbor.
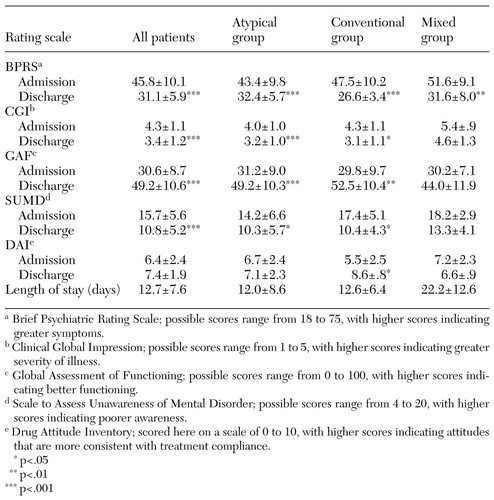 |
Table 1. Mean±SD scores on measures of symptoms, severity of illness, functional level, insight into illness, and attitudes toward medications in a sample of 36 state hospital patients at admission and discharge
1. Amador XF, Flaum M, Andreason NC, et al: Awareness of illness in schizophrenia and schizoaffective and mood disorders. Archives of General Psychiatry 51:826-836, 1994Crossref, Medline, Google Scholar
2. Coursey RD, Keller AB, Farrel EW: Individual psychotherapy and persons with serious mental illness: the client's perspective. Schizophrenia Bulletin 21:283-301, 1995Crossref, Medline, Google Scholar
3. Awad GA: Subjective response to neuroleptics in schizophrenia. Schizophrenia Bulletin 19:609-618, 1993Crossref, Medline, Google Scholar
4. Csernansky J: Risperidone vs halperidol for prevention of relapse in schizophrenia and schizoaffective disorders: a long-term double-blind comparison. Presented at the annual convention of the Society of Biological Psychiatry held in Washington, DC, May 13, 1999Google Scholar
5. Weiden PJ, Dixon L, Frances A, et al: Neuroleptic non-compliance in schizophrenia, in Advances in Neuropsychiatry and Psychopharmacology, vol 1. Edited by Tamminga C, Schulz SC. New York, Raven, 1991Google Scholar
6. Overall JE, Gorham DR: The Brief Psychiatric Rating Scale. Psychological Reports 10:799-812, 1962Crossref, Google Scholar
7. Guy W (ed): ECDEU Assessment Manual for Psychopharmacology. US Department of Health, Education, and Welfare Publication (ADM). Rockville, Md, National Institute of Mental Health, 1976Google Scholar
8. Weiler MA, Fleisher MH, McArthur-Campbell D: Insight and symptom change in schizophrenia and other disorders. Schizophrenia Research 45:29-36, 2000Crossref, Medline, Google Scholar
9. Kemp R, David A: Psychological predictors of insight and compliance in psychotic patients. British Journal of Psychiatry 169:444-450, 1996Crossref, Medline, Google Scholar
10. Greenfeld D, Strauss JS, Bowers MB, et al: Insight and interpretation of illness in recovery from psychosis. Schizophrenia Bulletin 15:245-252, 1989Crossref, Medline, Google Scholar



