Lithium Levels and Toxicity Among Hospitalized Patients
Abstract
OBJECTIVE: Although psychiatrists in the United States have used lithium for nearly 30 years, toxicity still occurs frequently. The authors report an attempt to reduce the incidence of lithium toxicity in hospitalized psychiatric patients and to identify factors associated with toxicity. METHODS: Serum lithium levels were monitored by the drug use evaluation committee at a psychiatric hospital between 1990 and 1996. Each laboratory result showing a serum lithium level of 1.5 mmol/L or more was promptly investigated, and the results were reported quarterly to the hospital staff association. RESULTS: The study found that in 6.8 percent of the 2,210 admissions during which lithium was administered, patients had serum levels of 1.5 mmol/L or higher. The number of excessive serum lithium levels decreased over the course of the study period. Only 27.8 percent of patients with excessive levels had signs and symptoms of toxicity. Of the excessive serum lithium levels that were investigated, 43.3 percent were detected in blood samples drawn at the time of admission. Women and elderly persons were significantly more likely to have excessive serum levels. Psychiatric diagnosis was not significantly associated with excessive serum levels. CONCLUSIONS: Education by the drug use evaluation committee may have helped to reduce the number of patients who experienced excessive lithium levels while hospitalized. Vigilance should be emphasized for women and elderly persons.
Lithium salts are commonly used in the pharmacotherapy of several psychiatric illnesses (1,2,3). Toxicity associated with lithium treatment is highly prevalent—75 to 90 percent of patients treated with lithium have signs or symptoms of toxicity at some point during their treatment (4). Many minor side effects may occur at serum levels of .6 to 1.2 mmol/L, although serious but reversible side effects can occur within this range as well (5,6,7,8). Side effects may be due to heightened sensitivity to the lithium ion or a disparity between serum and brain lithium concentrations. Severe toxic states, with or without prodromal symptoms, frequently occur at serum levels above 1.5 mmol/L (1). Neurological damage or death may occur when levels exceed 2.5 mmol/L (9).
Although a considerable literature has accumulated on lithium toxicity (4,10,11,12,13,14,15,16,17,18,19), few data are available on the monitoring of psychiatric inpatients and the role of a drug utilization evaluation committee in improving hospital practice to prevent lithium toxicity. Many hospitals have formed such committees to prevent medication-related problems such as lithium toxicity (20). We report the results of one such effort, using prospective data obtained for seven consecutive years as part of the work of a drug utilization evaluation committee at a psychiatric hospital. The study focused on identifying factors common to patients who had excessive lithium levels and the influence of the drug utilization evaluation committee in reducing the incidence of such toxicity.
Methods
The study was conducted from 1990 through 1996 by the drug utilization evaluation committee at a university-affiliated private psychiatric hospital. In an effort to reduce the incidence of lithium toxicity, the hospital had established a policy recommending that physicians check serum lithium levels on admission for patients known or suspected to be taking lithium before admission. In addition, the policy recommended that serum lithium levels be checked twice weekly during the hospitalization.
To identify all cases of lithium toxicity, the hospital's laboratory automatically reported every serum lithium level of 1.5 mmol/L or more to the treating physician and the pharmacy. The pharmacy in turn notified the physician member of the drug utilization evaluation committee (the first author), who promptly investigated the circumstances of the excessive level by reviewing the chart and interviewing the patient and the clinical staff treating the patient.
The following data were collected: patient's age and sex; diagnosis or indication for use of lithium; whether renal and thyroid function tests had been performed before the start of lithium treatment; presence of contraindications such as renal failure, vomiting, dehydration, blood urea nitrogen levels exceeding 5 mg/100 mL, serum creatinine levels exceeding 1.5 mg/100 mL, pregnancy, or breast-feeding; when the blood sample was obtained relative to time of admission; when lithium treatment was started; and changes in dosage. In addition, data were collected on the concomitant use of a diuretic, an angiotensin-converting enzyme inhibitor, a salt-free diet, or a regimen with three or more psychotropic medications; and whether the psychotropic medication regimen was changed more than twice within seven days of the detection of the excessive level. Also, adverse effects were noted, including lethargy, tremor, delirium, ataxia, polydipsia, and vomiting. Finally, the study recorded whether lithium was discontinued because of adverse effects or the excess serum lithium level.
The results of these investigations were summarized and reported every three months at a meeting of the hospital staff physicians. In addition, the drug use evaluation committee sent a letter to each treating physician involved in the care of a patient who had an excessive serum lithium level. The study reported here included every hospitalized patient with a serum lithium level of 1.5 mmol/L or higher during the study period. Chi square tests were used to test for statistical significance.
Results
From 1990 through 1996, we recorded a total of 2,210 admissions for which the patient received lithium during hospitalization. Serum lithium levels of 1.5 mmol/L or higher were observed in 151 of these admissions (6.8 percent). These levels ranged from 1.5 mmol/L to 2.98 mmol/L, with a mean±SD of 1.78±.29 mmol/ L. Table 1 presents the data by year. The proportion of excessive lithium levels in 1996 was significantly less than the proportion in 1990 (χ2=21.4, df=1, p<.001). Likewise, when the proportions of excessive lithium levels for 1990 and 1991 and those for 1992 through 1996 were combined, the latter group contained significantly fewer excessive lithium levels (χ2= 66.2, df=1, p<.001).
The mean±SD age of patients with excessive lithium levels was 45.2± 15.6 years. Of 851 admissions of patients aged 18 to 34 years who received lithium, excessive serum lithium levels were recorded in 48 cases (5.6 percent). Of 1,044 admissions of patients aged 35 to 64 years who received lithium, excessive levels were recorded in 81 cases (7.8 percent). Of 219 admissions of patients aged 65 years or older who received lithium, excessive levels were recorded in 22 cases (10 percent). Thus elderly persons were significantly more likely to have excessive lithium levels (χ2= 6.27, df=2, p<.05). Data on age were missing in 96 cases.
Of the 2,210 admissions during which lithium was administered, 1,200 were of female patients, and of these, 95 (7.9 percent) had an excessive serum lithium level. Of the 1,010 admissions during which lithium was administered to males, 56 (5.5 percent) had an excessive level. Females were significantly more likely than males to have an excessive level (χ2= 4.85, df=1, p<.05).
Table 2 summarizes the patients' primary axis I discharge diagnoses. When the distribution was compared for bipolar I disorder, psychotic spectrum disorder (schizophrenia, schizoaffective disorder, schizophreniform disorder, and psychosis not otherwise specified), and major depressive disorder, no significant differences were found. Thus the patients' diagnoses appeared to have no bearing on the likelihood of their having excessive lithium levels.
For the excessive lithium levels investigated in 1990 and 1991, the study did not record whether they were detected in blood samples drawn at the time of admission or later, during hospitalization. From 1992 through 1996, the study data included this information, and excessive levels were observed in the course of 60 hospitalizations. In 26 cases (43.3 percent), the high levels were found in blood samples drawn at the time of admission.
For the 151 admissions during which excessive lithium levels were found, 41 patients (27.2 percent) had signs and symptoms of lithium toxicity documented in the medical records. The most common manifestations of toxicity were ataxia (in 24 cases), lethargy (15 cases), delirium (six cases), polydipsia (six cases), vomiting (five cases), and tremor (three cases). Lithium was discontinued because of adverse effects in 24 cases (15.9 percent) and because of the detected excessive serum level in 134 cases (88.7 percent). In some cases, lithium was discontinued for both reasons.
Renal function tests were performed for all patients in whom excessive serum lithium levels were detected. Abnormally elevated levels of blood urea nitrogen or serum creatinine were observed in ten cases (6.6 percent). Diuretics were prescribed for patients during nine hospitalizations (6 percent), an angiotensin-converting enzyme inhibitor during four (2.6 percent), and a salt-free diet during three (2 percent). Polypharmacy consisting of at least two psychotropic medications in addition to lithium was observed in 32 cases (21.2 percent).
Discussion
As Table 1 shows, the number of excessive serum lithium levels dropped after the first two years. Although the drug use evaluation committee may have been responsible for this decline, many other factors could have accounted for this change, given the lack of randomization and systematic controls. During the last five years of the study an average of 3.9 percent of patients receiving lithium had excessive levels. However, 43.3 percent of these excessive levels were detected in blood samples drawn at the time of admission. It is possible that some patients attempted a "loading dose" of lithium just before admission in an attempt to recompensate and avoid hospitalization. Thus some or many of these excessive serum lithium levels may be due to ingestion of lithium shortly before the blood sample was drawn.
As for the 56.7 percent who suffered excessive lithium levels during hospitalization, it is hoped that continual monitoring, education, and feedback will further reduce this figure. Naturally it is important for hospital staff to draw blood samples for lithium level determinations before the morning dose of lithium is taken. Use of slow-release formulations of lithium also may help prevent excessive levels (21). Finally, it should be kept in mind that some patients suffering acute mania may require a lithium level as high as 1.5 mmol/L for therapeutic benefit.
Only 27.8 percent of inpatients with excessive lithium levels had signs and symptoms of toxicity, usually mild ataxia. The drug use evaluation committee's efforts have been directed in part to increasing vigilance to possible toxic side effects that might be misdiagnosed or overlooked. Additional efforts might now be directed to emphasizing the higher-risk groups, notably women and elderly persons.
Conclusions
The drug use evaluation process, with its continuing education and reinforcement for hospital staff, may have had a positive and sustained effect on the proportion of patients who had excessive lithium levels. In addition, the drug use evaluation committee defined specific groups at higher risk. These results appear to warrant maintaining the committee work.
The authors are affiliated with the department of psychiatry and human behavior at Brown University in Providence, Rhode Island. Send correspondence to Dr. Solomon, Mood Disorders Program, Department of Psychiatry, Rhode Island Hospital, 593 Eddy Street, Providence, Rhode Island 02903-4970 (e-mail, [email protected]).
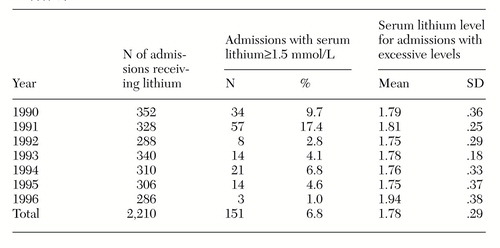 |
Table 1. Excessive lithium levels among 2,210 admissions to a psychiatric hospital, by year
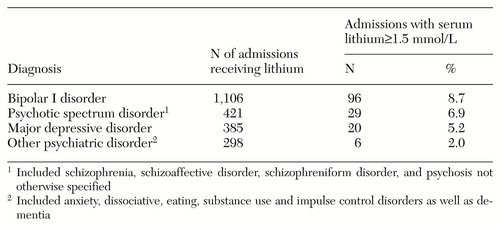 |
Table 2. Excessive lithium levels among 2,210 admissions, by diagnosis
1. Jefferson JW, Greist JH, Ackerman DL, et al: Lithium Encyclopedia for Clinical Practice, 2nd ed. Washington, DC, American Psychiatric Press, 1987Google Scholar
2. Mendels JJ, Secunda S: Lithium in Medicine. New York, Gordon & Breach, 1972Google Scholar
3. Johnson FN: The History of Lithium Therapy. London, MacMillan, 1984Google Scholar
4. Groleau G: Lithium toxicity. Emergency Medicine Clinics of North America 12:511-531, 1994Medline, Google Scholar
5. Speirs J, Hirsch SR: Severe lithium toxicity with "normal" serum concentrations. British Medical Journal 1:815-816, 1978Crossref, Medline, Google Scholar
6. Hay G, Simpson N: Neurotoxicity associated with therapeutic serum lithium levels. Lancet 2:160-161, 1982Crossref, Medline, Google Scholar
7. Bell AJ, Cole A, Eccleston D, et al: Lithium neurotoxicity at normal therapeutic levels. British Journal of Psychiatry 162:689-692, 1993Crossref, Medline, Google Scholar
8. Moscovich DG: Lithium neurotoxicity at normal therapeutic levels. British Journal of Psychiatry 163:410-412, 1993Crossref, Medline, Google Scholar
9. Janicak PG, Davis JM, Preskorn SH, et al: Principles and Practice of Psychopharmacotherapy. Baltimore, Williams & Wilkins, 1993Google Scholar
10. Okusa MD, Crystal LJT: Clinical manifestations and management of acute lithium intoxication. American Journal of Medicine 97:383-389, 1994Crossref, Medline, Google Scholar
11. Ramchandani D, Schindler BA: The lithium toxic patient in the medical hospital: diagnostic and management dilemmas. International Journal of Psychiatry in Medicine 23:55-62, 1993Crossref, Medline, Google Scholar
12. Schou M: Long-lasting neurological sequelae after lithium intoxication. Acta Psychiatrica Scandinavica 70:594-602, 1984Crossref, Medline, Google Scholar
13. Tueth MJ: Emergencies caused by side effects of psychiatric medications. American Journal of Emergency Medicine 12:212-216, 1994Crossref, Medline, Google Scholar
14. Simard M, Gumbiner B, Lee A, et al: Lithium carbonate intoxication: a case report and review of the literature. Archives of Internal Medicine 149:36-46, 1989Crossref, Medline, Google Scholar
15. Goddard J: Lithium intoxication. British Medical Journal 302:1267-1269, 1991Crossref, Medline, Google Scholar
16. Brown WT: The pattern of lithium side effects and toxic reactions in the course of lithium therapy, in Handbook of Lithium Therapy. Edited by Johnson FN. Baltimore, University Park Press, 1980Google Scholar
17. Smith RE, Helms PM: Adverse effects of lithium therapy in the acutely ill elderly patient. Journal of Clinical Psychiatry 43:94-99, 1982Medline, Google Scholar
18. Brumm VL, van Gorp WG, Wirshing W: Chronic neuropsychological sequelae in a case of severe lithium intoxication. Neuropsychiatry, Neuropsychology, and Behavioral Neurology 11:245-246, 1998Medline, Google Scholar
19. Kores B, Lader MH: Irreversible lithium neurotoxicity: an overview. Clinical Neuropharmacology 20:283-299, 1997Crossref, Medline, Google Scholar
20. Marken PA, Ezell JR: Criteria for use of lithium in adult inpatients and outpatients. Clinical Pharmacy 12:617-621, 1993Medline, Google Scholar
21. Kilts CD: The ups and downs of oral lithium dosing. Journal of Clinical Psychiatry 59(suppl 6):21-26, 1998Medline, Google Scholar



