Assessing Predictive Factors for Extended Hospitalization at Acute Psychiatric Admission
Abstract
OBJECTIVE: This study examined whether information obtained early in the hospitalization process can be used to assess a patient's need for extended care. METHODS: A sample of 2,430 inpatients who were admitted to a state psychiatric facility during a one-year index period (January through December 1997) were randomly assigned to a primary sample or a replication sample. Data were collected on demographic characteristics and history of previous hospitalization. The Brief Psychiatric Rating Scale-Anchored Version (BPRS-A) was administered to patients within 48 hours of admission, and four new subscales derived from ratings of newly admitted patients were calculated. Univariate and multivariate analyses were conducted to identify factors associated with whether a patient was discharged to the community or transported to another hospital for extended care. RESULTS: A discriminant analysis of the data correctly identified 70 percent of the patients who were referred for continued hospitalization and 80 percent of the patients who were discharged to the community. The main correlates of the need for extended inpatient services were, in descending order, scores on the BPRS-A resistance subscale, the number of previous referrals for extended hospitalizations, and scores on the BPRS-A positive symptoms and psychological discomfort scales. CONCLUSIONS: BPRS-A subscale scores should be considered to be at least as good as more traditional measures in predicting length of hospitalization.
With the advent of managed care, a premium has been placed on time-limited treatment in both inpatient and outpatient psychiatric settings. More effective psychotropic medications and a focus on symptom stabilization during hospitalization have resulted in a daily census decline and a reduction in the average length of stay at many psychiatric institutions (1). However, a subset of patients continues to use mental health resources to a disproportionate degree, as measured by length of hospitalization or repeated admissions over time (2,3,4).
This disproportionate use is problematic for two reasons. First, longer hospital stays do not necessarily mean better mental health care, improved social adjustment, diminished psychopathology, or fewer readmissions (5,6). This raises the question of why a cohort of patients continues to require extended hospitalization as well as the rationale for extending services when the utility of doing so is questionable. Second, given that patients with longer hospital stays generally also have more admissions (7) and longer previous admissions (8), questions have been raised as to whether these patients are receiving comprehensive mental health services provided in a competent manner.
In response to these concerns, researchers have focused on identifying demographic, psychiatric, and hospitalization variables that may be associated with high levels of service use. In general, the conclusions drawn from these studies are remarkably inconsistent (9). For example, when service use is defined as rehospitalization over a given period, the relationships between rate of rehospitalization and factors such as ethnicity, gender, age, employment, education, and socioeconomic status are equivocal (9,10,11,12,13,14,15). More support can be found for a relationship between psychiatric diagnosis and rehospitalization; individuals with schizophrenia or other psychoses are rehospitalized more often (11,12,16,17).
A secondary diagnosis of substance abuse or a comorbid personality disorder also appears to be associated with recidivism (11,14). Other patient variables related to recidivism include a greater number of previous hospitalizations (9,18,19,20), greater impairment in self-care skills (21), increased propensity toward violence (11,22), and greater medication noncompliance (9,23,24).
A considerable body of research has focused on the variables associated with length of hospital stay. The findings across these studies also are equivocal. For example, although some studies suggest that female patients are more likely to receive extended services (22,25), others have shown that demographic variables, including age, are poor predictors of length of stay (25,26,27,28).
Psychiatric diagnosis is a less convincing predictor of length of hospitalization than of recidivism. For example, some studies suggest that diagnosis is unrelated to length of stay (22,29,30), whereas others have found that individuals who have a diagnosis of a psychotic disorder are more likely to receive extended services (27,31,32). Moreover, axis II diagnoses (33), cognitive impairment (31,34), and coexistent substance use problems (31,32) have all been identified as correlates of length of stay. Other important variables may include homelessness (22,35), unemployment (31,36), marital status (8), social skill deficits (26), physical illness (37), patient resistance (22), use of electroconvulsive therapy or antipsychotic medication during hospitalization (31,38), type of insurance (39), and weather severity (40). It has been suggested that some of the discrepancies among these studies may be the result of several inherent methodological weaknesses (9), including underutilization of both descriptive and multivariate statistics and a lack of generalizability of findings because of nonrepresentative samples.
Given the inconsistencies in the literature, it is conceivable that alternative data, such as those obtained during the initial assessment in the hospital, may be more useful than "traditional" predictors in determining use of mental health services. For example, Swett (41) concluded that a higher score on the Brief Psychiatric Rating Scale (BPRS) (42,43)—particularly the thought disorder factor—predicted inpatient recidivism. Research that examines the usefulness of assessment data in predicting length of stay is sparse, although the utility of patient self-report measures (44), such as the Positive and Negative Syndrome Scale for schizophrenia (45) and the Scale for the Assessment of Negative Symptoms (46), show promise.
There also is some evidence to suggest that clinician-based measures, such as scores on the resistance and positive symptoms subscales of the BPRS (47), may account for significant variance in predicting length of stay (22). Although these preliminary results suggest that assessment data may be useful in identifying patients who are at risk of greater hospital use, further research is necessary to explore the robustness of the findings.
The study reported here was conducted to examine the relative utility of ratings on the BPRS-Anchored Version (BPRS-A) (48), demographic characteristics, and history of hospitalization in predicting within 48 hours of admission whether inpatients at a state psychiatric facility would be discharged to the community or transferred to another hospital for extended care at the end of their treatment at the facility. We selected extended care as a treatment outcome because it represented cases in which short-term care had unequivocally been inadequate.
To directly address the statistical criticisms outlined by Klinkenberg and Calsyn (9), we present descriptive data followed by multivariate analyses. Moreover, we used a large representative sample to enhance the generalizability of the results. The study variables were chosen on the basis of previous research that suggested that they are associated with greater hospital use and because these data could be obtained at admission. We hypothesized that BPRS-A ratings at admission would be more useful than traditional predictors in identifying patients who were at risk of needing extended care.
Methods
Participants
The sample consisted of 2,430 patients who were hospitalized during an index period of one year—January through December 1997—at the Harris County Psychiatric Center, a university-affiliated, 250-bed psychiatric hospital that serves the greater Houston metropolitan area. If a patient had multiple admissions during the index period, only the last admission was used in the data analyses. Table 1 presents the patients' demographic characteristics, history of hospitalization, and diagnosis and outcome at discharge.
The SPSS (version 10.0) randomization procedure was used to divide the sample into two subsets, a primary sample for derivation of a predictive model and a replication sample to test the stability of the results. Each subset contained a total of 1,215 patients, with an equivalent number of patients who required extended hospitalization (N=198) and patients who were discharged to the community (N=1,017).
Measures
The BPRS-A is a clinician-based rating instrument consisting of 18 items that describe dimensions of psychopathology. Items are rated on a 7-point scale ranging from "not present" to "very severe," with anchors in the form of behavior examples provided for each item's rating options. To be consistent with previous research (49), item responses were weighted from 1 to 7. The reliability and validity of the BPRS have been well documented across studies (50). Similarly, adequate interrater reliability has been demonstrated for BPRS-A total score at admission (47,48).
A recent psychometric analysis that included interrater reliability and scale validity supported the application of four factor-derived dimensions of the BPRS-A in acute inpatient settings (47). The four subscales are resistance, which has as its component items uncooperativeness, hostility, excitement, and grandiosity; positive symptoms, with the component items of unusual thought content, conceptual disorganization, hallucinatory behavior, suspiciousness, and disorientation; negative symptoms, with the component items of blunted affect, emotional withdrawal, and motor retardation; and psychological discomfort, with the component items of depressive mood, anxiety, somatic concern, guilt feelings, and tension.
Procedure
The BPRS-A was completed by one of 16 attending faculty psychiatrists within 48 hours of a patient's admission. Ratings were not based on a single interview, but rather represented a summary of all the information available after the patient had been admitted to the facility. Because the scale items are fundamental constructs of psychopathology that are assessed through a routine mental status assessment and a comprehensive interview (50), the attending psychiatrists received no formal training on the BPRS-A. Adequate reliability estimates for BPRS-A total score and factor scores at admission (Cronbach's alpha range=.68 to .80; N=1,556) and interrater reliability across pairs of attending psychiatrists and the residents assigned to them (range of intraclass correlation coefficients=.57 to .84, N=131) have been demonstrated in research conducted at the Harris County Psychiatric Center (47).
BPRS-A scores, demographic information, and hospitalization data for each patient were gathered daily from medical records and entered into a database.
Data analysis
Categorical data were analyzed with chi square analyses. Follow-up Fisher's exact tests were conducted on significant chi square analyses in the case of multiple levels of the independent variable—for example, marital status and ethnicity. For chi square analyses, effect sizes are reported with use of the phi statistic Φ (51) (small=.10, medium=.30, large=.50). Continuous dependent variables were examined by using one-way analyses of variance, with discharge placement as the independent variable.
For continuous data, estimated eta-squared (est. η2) (52) is presented as a measure of effect size (small=.01, medium=.06, large=.16). Variables that were demonstrated to be significantly different as a function of discharge status across both the primary and replication samples (conjoint p<.003) were retained for use in stepwise discriminant function analyses. This multivariate procedure was conducted to determine the relative value of variables established through replicated analyses in identifying patients who would subsequently need extended care. For these analyses, the F-to-remove statistic was used to determine the final set of variables. Standardized discriminant weights—that is, discriminant coefficients—are reported to indicate the relative value of variables to the discriminant function. In all stepwise regression analyses, data were tested to ensure that statistical assumptions were not violated. Box's M statistic was used to test the assumption of equal covariance matrices.
Results
Descriptive statistics for the entire sample and the two subsets—the primary sample and the replication sample—are presented in Table 2. Sixteen percent of the patients in the entire sample were transferred to extended care.
Univariate analyses
Demographic variables. Chi square analyses revealed a significant difference for marital status in both the primary sample (χ2=31.6, df=4, p<.001, Φ=.16) and the replication sample (χ2=21.43, df=4, p<.01, Φ=.13). In the primary sample, single patients were more likely to be transferred for extended care (χ2=47.7, df=1, p<.001), whereas those who were married (χ2= 26.5, df=1, p<.001), divorced (χ2=5.08, df=1, p<.05), or separated (χ2=4.45, df=1, p<.05) were more likely to be discharged to the community. Discharge status did not differ among widowed patients.
In the replication sample, the same pattern was evident. Single patients were more likely to be discharged to extended care (χ2=48.58, df=1, p<.001), and those who were married (χ2=23.43, df=1, p<.001), divorced (χ2=4.36, df=1, p<.05), or separated (χ2=4.21, df=1, p<.05) were more likely to be discharged to the community. Again, discharge status did not differ among widowed patients.
Discharge status among individuals in the primary sample differed as a function of gender (χ2=9.1, df=1, p<.01, Φ=.09), ethnicity (χ2=14.5, df=3, p<.05, Φ=.11), and employment history (χ2=11.2, df=1, p<.01, Φ=.10); however, these variables were not significantly associated with discharge status in the replication sample.
Hospitalization variables. In the primary sample, patients who were transferred for extended care had more previous admissions to the Harris County Psychiatric Center than patients who were discharged to the community (F=72.5, df=1, 1,213, p<.001, est. η2=.06). They also had more previous transfers for extended care (F=130.63, df=1, 1,213, p<.001, est. η2=.10). These findings held for the replication sample (F=64.21, df=1, 1,213, p<.001, est. η2=.05, and F=106.37, df=1, 1,213, p<.001, est. η2=.08, respectively).
Clinician ratings. As indicated in Table 2, patients in the primary sample who were transferred for extended care had higher BPRS-A total scores (F=54.74, df=1, 1,213, p<.001, est. η2=.04) and higher scores for resistance (F=155.12, df=1, 1,213, p<.001, est. η2=.11) and for positive symptoms (F=104.27, df=1, 1,213, p<.001, est. η2=.08). However, patients who had higher scores for psychological discomfort were more likely to be discharged to the community (F=21.30, df=1, 1,213, p<.001, est. η2=.02).
Analyses of the replication sample demonstrated the reliability of BPRS-A admission scores in predicting type of patient discharge. Patients who were transferred for extended care had higher total scores (F=81.19, df=1, 1,213, p<.001, est. η2=.06) and higher scores for resistance (F= 153.01, df=1, 1,213, p<.001, est. η2= .11) and positive symptoms (F= 136.97, df=1, 1,213, p<.001, est. η2= .11). Again, patients with higher scores for psychological discomfort were more likely to be discharged to the community (F=8.89, df=1, 1,213, p<.01, est. η2=.01).
Multivariate analyses
The final stage of data analysis involved examining the classificatory power of the three types of predictor variables—BPRS-A scores, demographic characteristics, and history of hospitalization—through stepwise discriminant function analyses. Only the six significant replicated variables were included in these analyses: marital status, dichotomized as single versus marital history; number of previous admissions to the Harris County Psychiatric Center; number of previous transfers for extended care; and scores on the BPRS-A subscales for resistance, positive symptoms, and psychological discomfort. Because of their shared variance with the factor scores, BPRS-A total scores were not included in these analyses.
The first analysis was conducted on the primary sample. All variables except number of previous admissions to the Harris County Psychiatric Center were retained (F= 63.53, df=5, 1,209, p<.001). In descending order of importance, the discriminant coefficients were BPRS-A resistance score (.52), number of previous transfers for extended care (.51), BPRS-A psychological discomfort score (-.37), BPRS-A positive symptoms score (.32), and marital status (-.13).
Four variables were replicated in the identical analysis conducted on the second sample (F=70.08, df=4, 1,210, p<.001). Number of previous admissions to the Harris County Psychiatric Center and marital status were not retained. In descending order of importance, the discriminant coefficients were BPRS-A resistance score (.48), BPRS-A positive symptoms score (.45), previous referrals for extended care (.44), and BPRS-A psychological discomfort score (-.30).
A final discriminant analysis was conducted on the entire sample and included the four variables that had been identified as robust predictors across both the primary and replication samples. These four variables were also found to be significant predictors in this final analysis (F=146.49, df=4, 2,425, p<.001); in descending order of importance, they were BPRS-A resistance score (.50), number of previous referrals for extended care (.49), BPRS-A positive symptoms score (.40), and BPRS-A psychological discomfort score (-.35). When this model was used, classification accuracy was 70 percent for extended hospitalization and 80 percent for community discharge. Overall classification accuracy was 78 percent.
Discussion
This study focused on outlining the relationship between the demographic, hospitalization history, and clinical variables assessed at patients' admission to a psychiatric hospital and the patients' need for continued hospitalization. The use of four predictor variables in a discriminant function analysis accurately predicted in 78 percent of the cases whether a patient would be discharged to the community or would require extended care. As there are no statistical guidelines to address the magnitude of the proportional chance versus predictive accuracy differential (53), the clinical significance of our model must be evaluated.
Eighty-four percent of the patients in the sample were discharged to the community after short-term treatment at the hospital; therefore, on the basis of chance alone, the probability that medical personnel would have predicted this outcome was 84 percent. Our model correctly predicted this outcome in 80 percent of the cases; therefore, the utility of the model for identifying this population was minimal.
However, on the basis of chance alone, the probability of clinicians' correctly predicting that a patient would be transferred for extended care was only 16 percent. In this case, the model's accurate prediction in 70 percent of the cases represents a dramatic improvement in the ability to identify these individuals at admission. The replicability of our findings across two samples, together with an almost fourfold increase over that expected by chance, supported the clinical significance of this model.
In this model, three of the four variables most highly associated with the need for extended care were subscale scores on the BPRS-A. Given that these scores accounted for greater variance in predicting extended care than more traditional predictors, this finding is provocative, and it has several potential implications. First, as researchers have acknowledged, a multitude of variables have been associated with high levels of service use (9,54). Even though our data were collected from a sizable patient sample, several variables associated with length of stay were found to be unreliable. Thus, in this area of research, the importance of using a replication paradigm has been demonstrated. To further explore the validity of the findings, the potential utility of BPRS-A subscales in predicting use of mental health services should be evaluated at other mental health facilities.
Second, many of the discrepancies among variables associated with extended care found in previous studies may reflect institution-specific differences in staff, treatment strategies, and the nature of aftercare services. The BPRS-A may provide standardized values that can help identify at-risk patients, regardless of treatment facility.
Third, considering the relative ease with which the BPRS-A can be integrated into clinical practice, this rating scale may be a practical and valuable screening tool when patients are admitted for acute care. It may be most valuable as a means of more efficiently targeting patients who need more intensive assessment as well as specialized therapeutic and pharmacological interventions. Fourth, because such patients also are most likely to return to the hospital (7), early identification may allow for more appropriate aftercare arrangements—for example, providing family education and ensuring medication compliance. Finally, the BPRS-A may be a particularly valuable predictive and diagnostic measure for patients who are admitted involuntarily or in a psychotic state and are thus unwilling or unable to cooperate in their own evaluation.
Conclusions
Use of the BPRS-A may improve patient assessment procedures and serve as a mechanism for facilitating more appropriate prerelease interventions and aftercare services (55). Whether use of the data obtained with the BPRS-A constitutes an improvement over the treating psychiatrist's unaided predictions is still a question that requires empirical study. Further investigation is necessary to explore the generalizability of our findings as well as the practicality of using BPRS-A data in a prospective manner to identify at-risk patients and to evaluate how early identification influences the selection of treatment strategies and whether such practices reduce the number of patients who need extended hospitalization.
The authors are affiliated with the University of Texas Houston Medical School and Harris County Psychiatric Center in Houston, Texas. Send correspondence to Dr. Lachar at the University of Texas Houston Medical School, Mental Sciences Institute, Department of Psychiatry and Behavioral Sciences, 1300 Moursund Avenue, Houston, Texas 77030-3497 (e-mail, [email protected]). An earlier version of this paper was presented at the annual meeting of the American Psychological Association held August 4-8, 2000, in Washington, D.C.
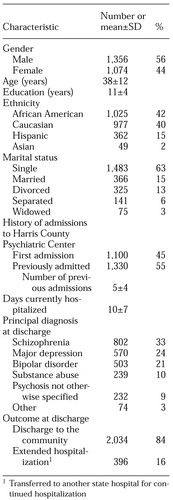 |
Table 1. Characteristics of 2,430 psychiatric in-patients in a study to predict the need for extended psychiatric hospitalization
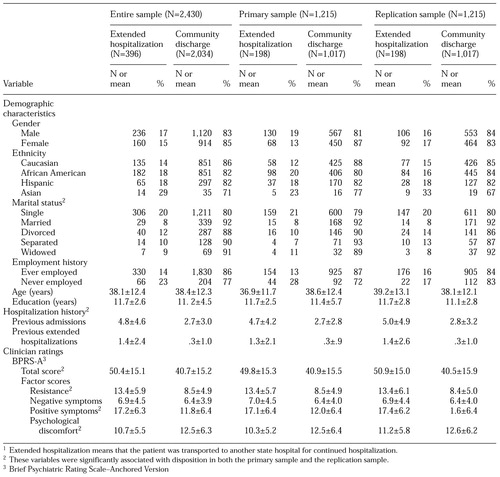 |
Table 2. Characteristics of patients at hospital admission, by whether they were subsequently transferred for extended hospitalization or discharged to the community1
1 Extended hospitalization means that the patient was transported to another state hospital for continued hospitalization
1. Mechanic D, McAlpine DD, Olfson M: Changing patterns of psychiatric inpatient care in the United States, 1988-1994. Archives of General Psychiatry 55:785-791, 1998Crossref, Medline, Google Scholar
2. Mojtabai R, Nicholson RA, Neesmith DH: Factors affecting relapse in patients discharged from a public hospital: results from a survival analysis. Psychiatric Quarterly 68:117-129, 1997Crossref, Medline, Google Scholar
3. Swett C: Symptom severity and number of previous psychiatric admissions as predictors of readmission. Psychiatric Services 46:482-485, 1995Link, Google Scholar
4. Wickizer TM, Lessler D: Do treatment restrictions imposed by utilization management increase the likelihood of readmission for psychiatric patients? Medical Care 36:844-850, 1998Google Scholar
5. Johnstone P, Zolese G: Systematic review of the effectiveness of planned short hospital stays for mental health care. British Medical Journal 318:1387-1390, 1999Crossref, Medline, Google Scholar
6. Mattes JA: The optimal length of hospitalization for psychiatric patients: a review of the literature. Hospital and Community Psychiatry 33:824-828, 1982Abstract, Google Scholar
7. Huntley DA, Cho DW, Christman J, et al: Predicting length of stay in an acute psychiatric hospital. Psychiatric Services 49:1049-1053, 1998Link, Google Scholar
8. Jakubaschk J, Waldvogel D, Wurmle O: Differences between long-stay and short-stay inpatients and estimation of length of stay: a prospective study. Social Psychiatry and Psychiatric Epidemiology 28:84-90, 1993Crossref, Medline, Google Scholar
9. Klinkenberg WD, Calsyn RJ: Predictors of receipt of aftercare and recidivism among persons with severe mental illness: a review. Psychiatric Services 47:487-496, 1996Link, Google Scholar
10. Sanguineti VR, Samuel SE, Schwartz SL, et al: Retrospective study of 2,200 involuntary admissions and readmissions. American Journal of Psychiatry 153:392-396, 1996Link, Google Scholar
11. Casper ES, Patsva G: Admission histories, patterns, and subgroups of the heavy users of a state psychiatric hospital. Psychiatric Quarterly 61:121-134, 1990Crossref, Medline, Google Scholar
12. Boydell KM, Malcolmson SA, Sikerbol K: Early rehospitalization. Canadian Journal of Psychiatry 36:743-745, 1991Crossref, Medline, Google Scholar
13. Kastrup M: Who became revolving door patients? Findings from a nationwide cohort of first time admitted psychiatric patients. Acta Psychiatrica Scandinavica 76:80-88, 1987Crossref, Medline, Google Scholar
14. Vogel S, Huguelet P: Factors associated with multiple admissions to a public psychiatric hospital. Acta Psychiatrica Scandinavica 95:244-253, 1997Crossref, Medline, Google Scholar
15. Snowden LR, Holschuh J: Ethnic differences in emergency psychiatric care and hospitalization in a program for the severely mentally ill. Community Mental Health Journal 28:281-291, 1992Crossref, Medline, Google Scholar
16. Fisher WH, Geller JL, Altaffer F, et al: The relationship between community resources and state hospital recidivism. American Journal of Psychiatry 149:385-390, 1992Link, Google Scholar
17. Rabinowitz J, Mark M, Popper M, et al: Predicting revolving-door patients in a 9-year national sample. Social Psychiatry and Psychiatric Epidemiology 30:65-72, 1995Crossref, Medline, Google Scholar
18. Monnely EP: Instability before discharge and previous psychiatric admissions as predictors of early readmission. Psychiatric Services 48:1584-1586, 1997Link, Google Scholar
19. Postrado LT, Lehman AF: Quality of life and clinical predictors of rehospitalization of persons with severe mental illness. Psychiatric Services 46:1161-1165, 1995Link, Google Scholar
20. Walker R, Minor-Schork D, Bloch R, et al: High risk factors for rehospitalization within six months. Psychiatric Quarterly 67:235-243, 1996Crossref, Medline, Google Scholar
21. Lyons JS, O'Mahoney MT, Miller SI, et al: Predicting readmission to the psychiatric hospital in a managed care environment: implications for quality indicators. American Journal of Psychiatry 154:337-340, 1997Link, Google Scholar
22. Averill PM, Hopko DR, Small D, et al: The role of psychometric data in predicting inpatient mental health service utilization. Psychiatric Quarterly 72:217-237, 2001Crossref, Google Scholar
23. Smith LD: Medication refusal and the rehospitalized mentally ill inmate. Hospital and Community Psychiatry 40:491-496, 1989Abstract, Google Scholar
24. Haywood TW, Kravitz HM, Grossman LS, et al: Predicting the "revolving door" phenomenon among patients with schizophrenic, schizoaffective, and affective disorders. American Journal of Psychiatry 152:856-861, 1995Link, Google Scholar
25. Sajatovic M, Donenwirth K, Sultana D, et al: Admissions, length of stay, and medication use among women in an acute care state psychiatric facility. Psychiatric Services 51:1278-1281, 2000Link, Google Scholar
26. Miller GH, Willer B: Length of hospitalization predicted by self-assessment of social competence. Journal of the Canadian Psychiatric Association 24:337-339, 1979Crossref, Medline, Google Scholar
27. Nieminen P, Isohanni M, Winblad I: Length of hospitalization in an acute patients' therapeutic community ward. Acta Psychiatrica Scandinavica 90:466-472, 1994Crossref, Medline, Google Scholar
28. Oiesvold T, Saarento O, Sytema S, et al: The Nordic comparative study on sectorized psychiatry: length of in-patient stay. Acta Psychiatrica Scandinavica 100:220-228, 1999Crossref, Medline, Google Scholar
29. Caton CL, Gralnick A: A review of issues surrounding length of psychiatric hospitalization. Hospital and Community Psychiatry 38:858-863, 1987Abstract, Google Scholar
30. McCrone P, Phelan M: Diagnosis and length of psychiatric inpatient stay. Psychological Medicine 24:1025-1030, 1994Crossref, Medline, Google Scholar
31. Herr BE, Abraham HD, Anderson W: Length of stay in a general hospital psychiatric unit. General Hospital Psychiatry 13:68-70, 1991Crossref, Medline, Google Scholar
32. Huntley DA, Cho DW, Christman J, et al: Predicting length of stay in an acute psychiatric hospital. Psychiatric Services 49:1049-1053, 1998Link, Google Scholar
33. Tucker P, Brems C: Variables affecting length of psychiatric inpatient treatment. Journal of Mental Health Administration 20:58-65, 1993Crossref, Medline, Google Scholar
34. Fulop G, Strain JJ, Fahs MC, et al: A prospective study of the impact of psychiatric comorbidity on length of hospital stays of elderly medical-surgical inpatients. Psychosomatics 39:273-280, 1998Crossref, Medline, Google Scholar
35. Kuno E, Rothbard AB, Averyt J, et al: Homelessness among persons with serious mental illness in an enhanced community-based mental health system. Psychiatric Services 51:1012-1016, 2000Link, Google Scholar
36. Munley PH, Devone N, Einhorn CM, et al: Demographic and clinical characteristics as predictors of length of hospitalization and readmission. Journal of Clinical Psychology 33:1093-1099, 1977Crossref, Medline, Google Scholar
37. Sloan DM, Yokley J, Gottesman H, et al: A five-year study on the interactive effects of depression and physical illness on psychiatric inpatient length of stay. Psychosomatic Medicine 61:21-25, 1999Crossref, Medline, Google Scholar
38. Creed F, Tomenson B, Anthony P, et al: Predicting length of stay in psychiatry. Psychological Medicine 27:961-966, 1997Crossref, Medline, Google Scholar
39. Hendryx MS, DeRyan J: Psychiatric hospitalization characteristics associated with insurance type. Administrative Policy and Mental Health 25:437-448, 1998Crossref, Medline, Google Scholar
40. Federman EJ, Drebing CE, Boisvert C, et al: Relationship between climate and psychiatric inpatient length of stay in veterans health administration hospitals. American Journal of Psychiatry 157:1669-1673, 2000.Link, Google Scholar
41. Swett C: Symptom severity and number of previous psychiatric admissions as predictors of readmission. Psychiatric Services 46:482-485, 1995Link, Google Scholar
42. Overall JE, Gorham DR: The Brief Psychiatric Rating Scale. Psychological Reports 10:799-812, 1962Crossref, Google Scholar
43. Overall JE, Gorham DR: The Brief Psychiatric Rating Scale (BPRS): recent developments in ascertainment and scaling. Psychopharmacology Bulletin 24:97-99, 1988Google Scholar
44. Galynker I, Cohen L, Salvit C, et al: Psychiatric symptom severity and length of stay on an intensive rehabilitation unit. Psychosomatics 41:114-120, 2000Crossref, Medline, Google Scholar
45. Kay SR, Fiszbein A, Opler LA: The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophrenia Bulletin 13:261-276, 1987Crossref, Medline, Google Scholar
46. Andreasen NC: The Scale for the Assessment of Negative Symptoms (SANS): conceptual and theoretical foundations. British Journal of Psychiatry 7:49-58, 1989Google Scholar
47. Lachar D, Bailley SE, Rhoades HM, et al: New subscales for an anchored version of the Brief Psychiatric Rating Scale: construction, reliability, and validity in acute psychiatric admissions. Psychological Assessment 13:384-395, 2001Crossref, Medline, Google Scholar
48. Woerner MG, Mannuzza S, Kane JM: Anchoring the BPRS: an aid to improved reliability. Psychopharmacology Bulletin 24:112-117, 1988Medline, Google Scholar
49. Lachar D, Bailley SE, Rhoades HM, et al: Use of BPRS-A percent change scores to identify significant clinical improvement: accuracy of treatment response classification in acute psychiatric inpatients. Psychiatry Research 89:259-268, 1999Crossref, Medline, Google Scholar
50. Faustman WO, Overall JE: Brief Psychiatric Rating Scale, in The Use of Psychological Testing for Treatment Planning and Outcome Assessment, 2nd ed. Edited by Maruish M. Mahwah, NJ, Lawrence Erlbaum, 1999Google Scholar
51. Cohen J: Statistical Power Analysis for the Behavioral Sciences, 2nd ed. Hillsdale, NJ, Lawrence Erlbaum, 1988Google Scholar
52. Keppel G: Design and Analysis: A Researcher's Handbook, 3rd ed. Englewood Cliffs, NJ, Prentice Hall, 1991Google Scholar
53. Hair JF, Anderson RE, Tatham RL, et al: Multivariate Data Analysis, 4th ed. Englewood Cliffs, NJ, Prentice Hall, 1995Google Scholar
54. Mezzich JE, Coffman GA: Factors influencing length of hospital stay. Hospital and Community Psychiatry 36:1262-1264, 1985Abstract, Google Scholar
55. Geller JL: Treating revolving-door patients who have "hospitalphilia": compassion, coercion, and common sense. Hospital and Community Psychiatry 44:141-146, 1993Abstract, Google Scholar