Datapoints: The Time Course of Treatment Costs Among Patients With Severe Mental Illness
Capitation presents unique problems in the severely mentally ill population, because treatment costs can run up to $125,000 per year. The financial viability of provider organizations can be threatened if they are assigned a disproportionate number of high-cost patients. Also, organizations can experience a strong incentive to undertreat or avoid high-cost patients.
One approach to decreasing undesirable incentives has been to adjust payments according to the risk of high future costs. A better understanding of the temporal course of treatment costs could inform contract design and help providers understand what to expect under risk contracts.
We analyzed data on treatment costs incurred by the Los Angeles County Department of Mental Health from 1988 to 1994. We studied 1,283 adults with severe mental illness who had received treatment for at least three of the past five years and who had annual treatment costs that averaged more than $20,000 per year.
The mean±SD annual treatment cost for these patients was $44,910± $25,489. As Figure 1 shows, 69 percent of costs resulted from hospital use and 21 percent from chronic care facilities. We inspected treatment costs for a subsample of patients for the entire five years. No recurring patterns were discernible. Indeed, the most striking features of the data were large changes in costs from year to year and numerous years with no treatment costs in between years with high costs. Figure 2 presents the average year-to-year change in annual treatment costs for each patient during the five years. The mean±SD change in annual treatment costs from one year to the next was $38,685±$37,364.
Developing useful risk adjustment models for the severely mentally ill population will be challenging and will likely require data on clinical predictors of hospitalization. Until substantial risk adjustment is possible, policy makers using capitation should strongly consider blended payment schemes that combine risk adjustment with mechanisms such as corridors of risk or partial fee-for-service payments (1).
Acknowledgments
This research was supported by the Department of Veterans Affairs and the UCLA-Rand Research Center on Managed Care for Psychiatric Disorders.
Dr. Young is associate director of the Mental Illness Research, Education, and Clinical Center in the Department of Veterans Affairs Veterans Integrated Service Network 22, 11301 Wilshire Boulevard, Los Angeles, California 90073. Dr. Kapur is an associate economist at Rand in Santa Monica, California. Mr. Murata is district chief of the Los Angeles County Department of Mental Health. Harold Alan Pincus, M.D., and Terri L. Tanielian, M.A., are editors of this column.
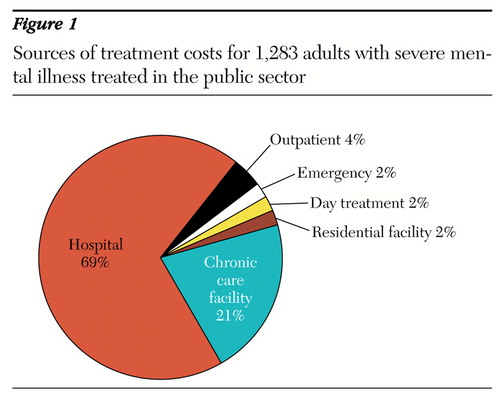
Figure 1. Sources of treatment costs for 1,283 adults with severe mental illness treated in the public sector
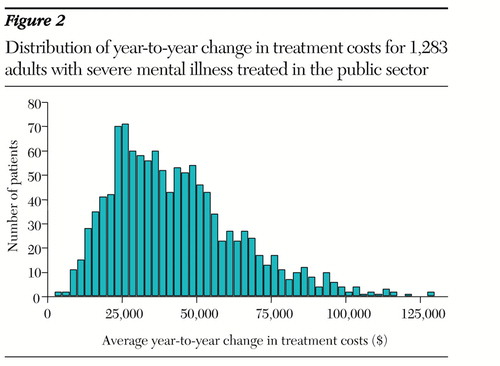
Figure 2. Distribution of year-to-year change in treatment costs for 1,283 adults with severe mental illness treated in the public sector
1. Newhouse JP: Risk adjustment: where are we now? Inquiry 35:122-131, 1998Google Scholar



