Age at First Alcohol Use: A Risk Factor for the Development of Alcohol Disorders
Abstract
OBJECTIVE: This study aimed to describe the natural course of DSM-III-R alcohol disorders as a function of age at first alcohol use and to investigate the influence of early use as a risk factor for progression to the development of alcohol disorders, exclusive of the effect of confounding influences. METHOD: Data were obtained from a community sample (N=5,856) of lifetime drinkers participating in the 1990–1991 Mental Health Supplement of the Ontario Health Survey.RESULTS: Survival analyses revealed a rapid progression to alcohol-related harm among those who reported having their first drink at ages 11–14. After 10 years, 13.5% of the subjects who began to drink at ages 11 and 12 met the criteria for a diagnosis of alcohol abuse, and 15.9% had a diagnosis of dependence. Rates for subjects who began to drink at ages 13 and 14 were 13.7% and 9.0%, respectively. In contrast, rates for those who started drinking at ages 19 and older were 2.0% and 1.0%. Unexpectedly, a delay in progression to harm was observed for the youngest drinkers (ages 10 and under). Hazard regression analyses revealed a nonlinear effect of age at first alcohol use, marked by an elevated risk of developing disorders among subjects first using alcohol at ages 11–14. CONCLUSIONS: First use of alcohol at ages 11–14 greatly heightens the risk of progression to the development of alcohol disorders and therefore is a reasonable target for intervention strategies that seek to delay first use as a means of averting problems later in life.
In many societies the use of alcohol during the teenage and young adult years is a common phenomenon. For large numbers of youth it may signify nothing more than healthy psychological experimentation (1). It is also true that many drinkers reduce their consumption in early adulthood to conform to the expectations and obligations of adult social roles such as marriage, childbearing, and employment (the role-incompatibility theory) (2). However, epidemiological data have shown that a substantial minority of lifetime alcohol users (20%–50%) progress to one or more alcohol problems or become alcohol dependent (3). The social, economic, and health-related costs associated with these conditions are enormous. In the United States, the total economic costs alone of alcohol disorders for 1990 was estimated at $98.6 billion (4).
A potentially powerful predictor of progression to alcohol-related harm is age at first use. Evidence suggests that the earlier the age at which young people take their first drink of alcohol, the greater the risk of abusive consumption (5) and the development of serious problems, including alcohol disorders (6, 7). In the United States, Grant and Dawson’s analysis (8) of the National Longitudinal Alcohol Epidemiological Survey found that over 40% of all individuals who reported drinking alcohol before the age of 14 became alcohol dependent, four times the rate (10%) observed for those who first reported drinking at ages 20 and older.
Explanations concerning why early alcohol use increases the risk of later alcohol problems are varied. Some experts assert that early use interferes with important cognitive and social learning processes that determine healthy social functioning in later life (9). Others suggest that early use is simply a correlate of some unknown condition or circumstance (e.g., childhood psychiatric disorder) that is causally related to the manifestation of alcohol problems (10). A third position suggests that using alcohol in early adolescence increases the vulnerability to subsequent alcohol problems because it occurs at a time when environmental conditions (e.g., onset of puberty and concerns regarding the opinions of one’s peers) strongly support continued and more regular use (11, 12).
Unfortunately, investigations of the effect of age at first alcohol use on the development of alcohol problems have been limited in several respects. One shortfall is the failure to control for the confounding influence of time. Young drinkers are, on average, exposed to the risk for developing problems for a longer period. As a result, time since first use of alcohol rather than age at first use may be the more important predictor of progression to alcoholism (13). Another shortfall concerns the absence of appropriate controls. Characteristics such as sex, racial or ethnic affiliation, biological factors (e.g., early puberty), involvement with delinquent peers, childhood conduct problems, as well as early adverse life events or circumstances not only influence the age at which young people take their first drink of alcohol but also the risk of developing problems with alcohol in the adult years (14, 15). When these potential confounding influences are not held constant, the effect of age at first alcohol use may be overstated.
From a public health perspective, a systematic study of the effects of age at first alcohol use is important. Prevention programs that are effective in delaying how early young people begin using alcohol have the potential for negating later problems, thereby reducing individual suffering and averting social, economic, and health-related costs at the societal level. The urgency of implementing effective programs is underscored by recent trends indicating a steady decline in the average age at first alcohol use (16, 17).
This article has two main objectives. The first is to describe the natural course of DSM-III-R alcohol disorders in the general population for different categories of age at first use of alcohol. A second objective is to investigate the influence of age at first use on the risk of progressing to disorders, holding potential confounding factors constant.
Method
Sample
Data were obtained from the 1990–1991 Ontario Mental Health Supplement (18), a stratified, multistage, area probability sample of the Ontario household population aged 15 and over. Excluded were residents of First Nations Peoples’ reserves, inmates, foreign service personnel, and residents of remote areas. The sample represented a 9,953-case subset that was randomly selected from the household interview portion of the 1990 Ontario Health Survey, a general health survey of over 60,000 Ontario residents. Eligible respondents from the Ontario Mental Health Supplement numbered 35,690, corresponding to a total of 14,478 eligible households from the third and fourth quarters of the Ontario Health Survey data collection. Participating households numbered 13,002; one individual was randomly selected from each. Of this number, 9,953 agreed to participate, resulting in a response rate of 76.5%. An analysis of supplement respondents and nonrespondents found little or no difference between groups on key measures of health status, employment, income, and marital status (19).
Measurement
Information on alcohol use and alcohol disorders was obtained by using a modified version of the World Health Organization’s Composite International Diagnostic Interview (20). The modified version of the Composite International Diagnostic Interview is a structured diagnostic interview for field interviewers without any formal clinical training that is designed to generate DSM-III-R and ICD-10 diagnoses. DSM-III-R diagnoses contained in the Ontario Mental Health Supplement that were assessed by means of the Composite International Diagnostic Interview include substance, mood, and anxiety disorders; antisocial personality disorder; and bulimia. Also included were questions on childhood events and circumstances, parental mental illness, and other family background characteristics, as well as questions regarding service use. Administration of the Composite International Diagnostic Interview was carried out by trained interviewers employed by the Special Surveys Group at Statistics Canada. Reliability and validity analysis of the Composite International Diagnostic Interview has indicated good test-retest and interrater reliability and acceptable levels of validity for most DSM-III-R lifetime diagnoses, including drug disorders (21, 22).
The dependent variable in this study was the occurrence of a lifetime alcohol disorder (abuse or dependence) in the time period since age at first alcohol use. Right-censored cases included individuals who had not experienced the event of interest (alcohol disorder) by the time of the interview. Respondents eligible to answer questions pertaining to symptoms of abuse or dependence included those who reported having had 12 or more drinks of alcohol over a 1-year period during their lives.
According to DSM-III-R, lifetime alcohol abuse is defined as a maladaptive pattern of alcohol use indicated by continued use, despite a persistent or recurrent social, occupational, psychological, or physical problem that is caused or exacerbated by drug use or by recurrent use in physically hazardous situations. Individuals must never have met the criteria for a diagnosis of alcohol dependence. Lifetime alcohol dependence is defined as membership in at least three of nine different alcohol-related symptom categories. For abuse and dependence, symptoms must have persisted for at least 1 month or have occurred repeatedly over a longer period (for more details, see DSM-III-R).
Age at onset of lifetime alcohol dependence referred to the age at which a respondent experienced a third alcohol symptom. Age at first drink of alcohol was defined as follows: “Not counting sips, how old were you the very first time you had a drink of beer, wine, or liquor?”
The following variables were identified as having a possible confounding influence on the relationship between age at first alcohol use and progression to the development of alcohol disorders.
1. Respondent’s demographic and socioeconomic background characteristics (sex, age cohort, childhood place of residence [rural area, small town, or city], ethnic affiliation [British/German/Dutch, French, Southern European, Canadian, or other], number of childhood siblings, childhood family dependence on welfare, and childhood parental education while growing up [primary, secondary, or postsecondary]).
2. Childhood conduct problems (involvement with juvenile justice system, overnight stay in jail or detention center, violent behavior, or property offenses).
3. Negative childhood life events (frequent geographic moves, failure in school, parental death, or parental separation).
4. Childhood family strain (physical abuse, sexual abuse, absence of a close or confiding relationship with at least one adult, parental conflict, parental alcohol and drug abuse, or parental mania, depression, or schizophrenia).
Statistical Analysis
The Kaplan-Meier survivorship function (23) was used to estimate the probability of not developing an alcohol disorder for each year in the sample for which there was at least one case of alcohol disorder. This method has the advantage of estimating year-by-year probabilities of developing an alcohol disorder while controlling for elapsed time. We chose to focus on the complement of this function—the cumulative failure rate, which is defined as the cumulative probability of developing an alcohol disorder at successive intervals of time since entering the alcohol-use state (having a first drink). Cumulative failure curves were estimated by collapsed categories for age at first alcohol use, with significant differences assessed by using the log-rank statistic.
Because time was measured in discrete units (i.e., years), multivariate, discrete-time hazard regression analysis was used to model predictors of the progression to developing an alcohol disorder. To estimate this model, the original data sets, containing one record per person, were transformed into person-year files, with one record for each year that each person was observed or followed (for more details, see reference 24). A series of dummy variables was created to denote the time period to which each record corresponded. A dichotomous event indicator was also created to indicate whether the event of interest (e.g., an alcohol disorder) occurred in the last year a person was observed. Thus, a person who progressed to the development of an alcohol disorder after 10 years in the alcohol-use state would have received a 0 on the event indicator for the first nine records and a 1 for the tenth record, indicating progression. In contrast, a person observed for 10 years who did not experience a disorder by the time of the survey (i.e., a right-censored case) would have received a 0 on the first nine records and a 0 on the tenth.
After data conversion, SAS logistic regression (25) was applied to the person-year data. The event indicator (e.g., coded as 1 for an alcohol disorder or 0 for absence of a disorder) was regressed on the set of time dummy variables and the set of hypothesized predictors. Information on main effects was given by the odds ratio and the Wald statistic, indicating the contribution of individual predictors to model fit. The significance of estimated odds ratios was judged by using a two-tailed t test derived by dividing the unstandardized coefficient by its standard error.
To avoid inflated tests of significance, sample weights were applied to the data and rescaled to equal the actual number of respondents in the sample. These weights accounted for all relevant features of the sampling design, including unequal probabilities of selection, nonresponse (person and household level), and an adjustment to align the age and sex distribution of the sample with the age and sex distribution of the population. To adjust for multiple testing in our multivariate models, only results significant at p<0.01 were reported.
Results
Among 5,856 lifetime drinkers in our study, 8.6% (N=501) recorded an age at onset of alcohol abuse (median age=17.70 years); 8.1% (N=473) recorded an age at onset of alcohol dependence (median age=20.40 years). The estimated median age at first drink of alcohol was 15.24 years.
Figure 1 shows that the groups at greatest risk of developing alcohol abuse included subjects who started to drink at ages 11–14. Ten years after their first drink 13.5% (49 of 363) of the respondents ages 11 and 12 and 13.7% (155 of 1,129) of the respondents ages 13 and 14 had progressed to a diagnosis of alcohol abuse, compared to just 2.0% in the reference group (19 and older) (18 of 920). The risk of developing alcohol abuse for the earliest to start drinking (younger than age 11) was well below that observed for most other groups until 10 years after the first drink. After this point the risk profile climbed steadily, reaching a high of 13% after 20 years. In Table 1, model A, respondents who had their first drink at age 13 or 14 or younger were four to five times more likely to develop alcohol abuse than subjects in the reference group. However, the adjusted results (model B) reveal a nonlinear effect. Vulnerability to the risk of abuse is highest for the pre- and early adolescents who started drinking (ages 11–14), followed by the earliest to start drinking (younger than age 11) and the subjects having their first drink at age 15 or 16.
Figure 2 shows that the highest risk profile for developing lifetime alcohol dependence occurred for subjects who had their first drink at age 11 or 12. Ten years after their first drink, 15.9% (57 of 359) of the respondents in this age group qualified for a diagnosis of lifetime alcohol dependence compared to 1.0% (9 of 920) of those ages 19 and older. Unlike the results for alcohol abuse, the risk for alcohol dependence for those having their first drink at age 13 or 14 (9.0%, 102 of 1,130) was well below the risk for those starting to drink at age 11 or 12. The risk profile for the earliest drinkers (younger than age 11) bears a close similarity to the profile on alcohol abuse. In the first 6 years after the first drink, the risk of dependence remains low. After 7 years it begins to climb, and by 10 years it exceeds the risk for most other age groups (except ages 11 and 12). Results in Table 1, model A, show that those who started to drink at age 11 or 12 were nearly 10 times more likely than those who started drinking later (ages 19 and older) to become alcohol dependent. The next highest rate occurs for those starting to drink before age 11, followed by those starting to drink at age 13 or 14. Adjusted results (model B) show that the risk of developing dependence for those starting to drink at ages 15–18 is not significant (relative to the reference group). The highest risk occurs for subjects ages 11–14, followed by the youngest subjects starting to drink.
Discussion
The objective of this study was twofold: 1) to describe the natural course of alcohol disorders for different categories of age at first alcohol use in a general population setting, and 2) to examine the extent to which age at first alcohol use exerts a unique influence on the risk of developing alcohol disorders, holding potential confounding factors constant.
Our work has shown that individuals who begin using alcohol in the pre- and early adolescent years (ages 11–14) are most vulnerable to the risk of developing DSM-III-R alcohol disorders. Unexpectedly, the highest risk profiles did not occur for the earliest starters. Having a first drink before the age of 11 did not elevate the risk of developing an alcohol disorder for 6 years after initiating use. In fact, during this period, the risk profile for the earliest starters did not differ significantly from the profile observed for very late starters (ages 19 or older). It was not until 6–8 years after starting to drink that the distinctive risk characteristics became firmly crystallized; then a rapid upward progression to disorders occurred that cut across most other age-at-onset profiles. This nonlinear effect was maintained in our multivariate models, which held confounding influences constant.
Given the Ontario Mental Health Supplement’s use of retrospective data as a means of reconstructing drug use histories, a cautious interpretation of the results is required. Some respondents may have forgotten when drug-related events occurred, they may have distanced the age of their first drink, or they may have telescoped drug-related events. Distortions of the timing of past drug-related events are likely to occur with greater frequency among certain groups, particularly those experiencing drug-related problems at the time of the interview and members of older age cohorts. Underreporting or overreporting of events, which vary systematically with respondent sociodemographic characteristics, may lead to biased parameter estimates. Retrospective surveys are also affected by selectivity bias since respondents may not be totally representative of past cohorts. Some would have died or migrated in the past; they therefore would not have been part of the survey population. Since the less healthy and geographically mobile may have a greater propensity to start using drugs early (or progress to serious abuse), underestimation of continuity in drug use behavior may result. A related issue pertains to coverage error. The focus of the Ontario Mental Health Supplement on permanent residential dwellers excluded a number of at-risk populations, such as aboriginal groups, homeless people, inmates, and patients residing in psychiatric institutions. The inclusion of these groups would have resulted in a slightly higher prevalence rate of lifetime alcohol disorders.
Other limitations pertain to measurement. Since DSM-III-R did not require a clustering of symptoms to qualify for a diagnosis of lifetime dependence, age at onset of dependence was defined as the age at which a respondent experienced the third criterion A symptom and met the criterion B requirement of persistence. This measure is somewhat less than ideal since it is unclear whether individuals who reached the third symptom were still positive on the first or second. Our study would have also benefited from more detailed alcohol history data in the time between the first use of alcohol and onset of abuse and dependence. Information on the number of episodes of heavy drinking, number and length of spells of no alcohol use, and age when first feeling drunk from the effects of alcohol is required to fully understand the processes that lead to the development of alcohol disorders.
With these limitations in mind, we believe this study has uncovered important information concerning the influence of early alcohol use on the risk of the development of DSM-III-R alcohol disorders. The most unique finding is the nonlinear form of the relationship between age at first drink and the risk of alcohol-related harm (specifically, the significant delay in the development of alcohol abuse and dependence among those who had their first drink before the age of 11 and the elevated risk of experiencing disorders—in particular, alcohol dependence—among those first using alcohol at age 11 or 12). In the United States, Grant and Dawson (8) made a similar finding but did not make formal mention of it in the report of their results. For example, they found a prevalence rate for alcohol abuse of 8.3% among those starting to drink at age 12 and younger, which is only marginally different from the 7.8% they reported for those starting to drink alcohol at age 18 (but well below the 11.5% reported for subjects starting to drink at age 13). These differences might have been even larger had the authors chosen to separate respondents beginning to drink at age 11 or 12 from earlier starters.
The significant delay in progression to the development of alcohol disorders observed among the earliest starters (younger than age 11) may be a function of a concerted effort by significant others (e.g., parents or teachers) to prevent the occurrence of further use. This reasoning is based on the idea that the progression to alcohol-related harm is partially governed by societal norms and expectations that dictate the appropriate age at which youth may engage in contested behaviors, including the legal use of substances (26). First alcohol use that arrives well ahead of the “social clock” set by society for contested behaviors is likely to provoke a swift response. A second explanation is that young people who use alcohol very early are less likely to have access to large quantities, a factor that might explain the rapid progression to disorders beginning around 6 years after the first drink, a time when most would have entered their adolescent years and become exposed to peer-related influences (i.e., a greater availability of alcohol and more pressure to use). This interpretation draws some support from studies of tobacco use. Breslau and associates’ study of nicotine dependence in the Detroit area (27) found that compared to late starters, early tobacco starters (under age 14) possessed a longer lag time to daily smoking (possibly resulting from a lack of environmental conditions to support frequent use or an age-related displeasure for the taste and experience of smoking) that served to reduce their risk of progression to nicotine dependence. Finally, children belonging to many southern European ethnic groups (e.g., those of Italian and Portuguese descent) consume alcohol as part of normal meal-time activities. Consumption is considered the norm within these contexts and thus is less likely to lead to the development of problems (at least in the short term).
The identification of the pre- and early adolescent years as a highly vulnerable period of risk for the development of alcohol-related harm deserves attention. Between ages 11–14 children experience a variety of social and psychological changes (e.g., self-concept formation and the acquisition of learned social skills) that are instrumental for healthy social functioning at a later age. The initiation of alcohol use during this critical time may interfere with these processes, causing an escalation toward heavier and more frequent consumption. Pre- and early adolescent children are also undergoing significant life transitions, including puberty and entry into high school. Research has shown that these transitions constitute a source of acute anxiety and stress, giving rise to a variety of academic and behavioral problems (28). Children who begin using drugs in the context of experiencing these life stressors are known to adopt continued and more frequent alcohol use as a strategy of coping with their problems (29).
This study raises important policy implications for the development of alcohol-abuse prevention programs for youth. The results demonstrate that prevention programs that are effective in delaying alcohol use until age 15 or 16 or later will avert substantial alcohol-related harm in later life. However, the success of these prevention efforts may depend on the knowledge of how early use influences problem development. We suggested a number of pathways, including the interruption of key learning processes and the adoption of inappropriate strategies (i.e., frequent alcohol use) to cope with an accumulation of environmental stressors during the late childhood and early adolescent years. Future research involving longitudinal data is required to test these linkages. Additional work should also be carried out to determine if the patterns of association between early alcohol use and later problems observed here also apply to other drugs. Finally, our finding of a significant delay in progression to the development of alcohol-related harm among the earliest starters (under age 11) requires further study. Future investigators may need to distinguish between the initiation of alcohol use in the context of the home (where children may have limited access to alcohol or where early use is culturally accepted among some groups) and the initiation of use outside the home, in the context of one’s relationship with peers, where consumption may be more closely tied to the development of problems.
 |
Received May 3, 1999; revision received Sept. 23, 1999; accepted Dec. 10, 1999. From the Social, Prevention and Health Policy Research Department, Centre for Addiction and Mental Health, London and Toronto; the Canadian Centre for Studies of Children at Risk, Hamilton Health Sciences Corporation, Hamilton, Ontario; and the Faculty of Health Sciences, Chedoke-McMaster University, Hamilton, Ontario. Reprints are not available. Address correspondence to Dr. DeWit, Social, Prevention and Health Policy Research Department, Centre for Addiction and Mental Health, 100 Collip Circle, Suite 200, London, Ontario N6G 4X8, Canada; [email protected] (e-mail).
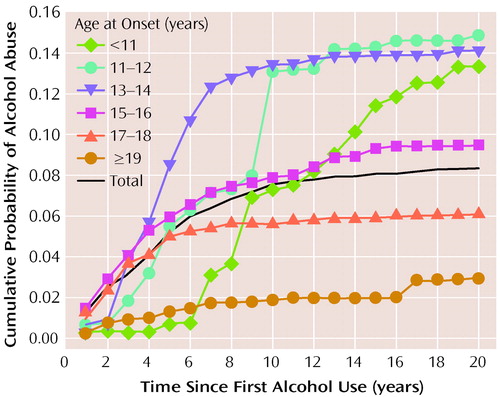
Figure 1. Probability of Lifetime Alcohol Abuse Among 5,856 Lifetime Drinkers, by Time Since First Use and Age at First Usea,b
aLog-rank statistic=99.19, df=5, p<0.001.
bOf the 5,856 lifetime drinkers, 501 developed lifetime alcohol abuse.

Figure 2. Probability of Lifetime Alcohol Dependence Among 5,856 Lifetime Drinkers, by Time Since First Use and Age at First Usea,b
aLog-rank statistic=249.89, df=5, p<0.001.
bOf the 5,856 lifetime drinkers; 473 developed alcohol dependence.
1. Shedler J, Block J: Adolescent drug use and psychological health. Am Psychol 1990; 45:612–630Crossref, Medline, Google Scholar
2. Yamaguchi K, Kandel DB: On the resolution of role incompatibility: a life event history analysis of family roles and marijuana use. AJS 1985; 90:1284–1325Google Scholar
3. Helzer JE, Canino GJ: Alcoholism in North America, Europe, and Asia. New York, Oxford University Press, 1992Google Scholar
4. Rice DP: The economic cost of alcohol abuse and dependence:1990. Alcohol Health and Research World 1993; 17:10–11Google Scholar
5. Hawkins JD, Graham JW, Maguin E, Abbott R, Hill KG, Catalano RF: Exploring the effects of age of alcohol use initiation and psychosocial risk factors on subsequent alcohol misuse. J Stud Alcohol 1997; 58:280–290Crossref, Medline, Google Scholar
6. Chou SP, Pickering RP: Early onset of drinking as a risk factor for lifetime alcohol-related problems. Br J Addict 1992; 87:1199–1204Google Scholar
7. Gruber E, DiClemente RJ, Anderson MM, Lodico M: Early drinking onset and its association with alcohol use and problem behavior in late adolescence. Prev Med 1996; 25:293–300Crossref, Medline, Google Scholar
8. Grant BF, Dawson DA: Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: results from the National Longitudinal Alcohol Epidemiological Survey. J Subst Abuse 1997; 9:103–110Crossref, Medline, Google Scholar
9. Clayton RR: Transitions in drug use: risk and protective factors, in Vulnerability to Drug Abuse. Edited by Glantz M, Pickens R. Washington, DC, American Psychological Association, 1992, pp 15–51Google Scholar
10. Robins LN, Przybeck TR: Age of onset of drug use as a factor in drug and other disorders. NIDA Res Mongr 1985; 56:178–192Medline, Google Scholar
11. Guthrie BJ, Loveland-Cherry C, Frey MA, Dielman TE: A theoretical approach to studying health behaviors in adolescents: an at-risk population. Fam Community Health 1994; 17:35–48Crossref, Google Scholar
12. Zucker RA, Fitzgerald HE: Early developmental factors and risk for alcohol problems. Alcohol Health and Research World 1991; 15:18–24Google Scholar
13. Yamaguchi K: Drug use and its social covariates from the period of adolescence to young adulthood: some implications from longitudinal studies, in Recent Developments in Alcoholism, vol 8. Edited by Galanter M. New York, Plenum Press, 1990, pp 125–143Google Scholar
14. Hawkins JD, Catalano RF, Miller JY: Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychol Bull 1992; 112:64–105Crossref, Medline, Google Scholar
15. Hawkins JD, Arthur MW, Catalano RF: Preventing substance abuse, in Building a Safer Society: Strategic Approaches to Crime Prevention. Edited by Farrington D, Tonry M. Chicago, University of Chicago Press, 1995, pp 343–428Google Scholar
16. Johnston LD, O’Malley PM, Bachman JG: National Survey Results on Drug Use From the Monitoring the Future Study, 1975–1995. Rockville, Md, National Institute on Drug Abuse, 1997Google Scholar
17. National Study on Substance Use Among Women in the United States. Rockville, Md, Substance Abuse and Mental Health Services Administration, Office of Applied Studies, 1997Google Scholar
18. Ontario Health Survey 1990, Mental Health Supplement: User’s Manual, vol 1: Documentation. Toronto, Ontario Ministry of Health, 1995Google Scholar
19. Boyle MH, Offord DR, Campbell D, Catlin G, Goering P, Lin E, Racine Y: Mental health supplement to the Ontario Health Survey: methodology. Can J Psychiatry 1996; 41:549–558Crossref, Medline, Google Scholar
20. World Health Organization: Composite International Diagnostic Interview (CIDI), version 1.0. Geneva, WHO, 1990Google Scholar
21. Wittchen H-U: Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res 1994; 28:57–84Crossref, Medline, Google Scholar
22. Wittchen H, Burke JD, Semler G, Pfister H, Von Cranach M, Zaudig M: Recall and dating of psychiatric symptoms. Arch Gen Psychiatry 1989; 46:437–443Crossref, Medline, Google Scholar
23. Efron B: Logistic regression, survival analysis, and the Kaplan-Meier curve. J Am Statistical Assoc 1988; 83:414–425Crossref, Google Scholar
24. Singer JD, Willett JB: It’s about time: using discrete-time survival analysis to study duration and the timing of events. J Educational Statistics 1993; 18:155–195Google Scholar
25. SAS/STAT User’s Guide, version 6, 4th ed, vol 2. Cary, NC, SAS Institute, 1989Google Scholar
26. Paglia A, Room R: How unthinkable and at what age? adult opinions about the social clock of contested behaviours by teenagers. J Youth Studies 1998; 1:295–314Crossref, Google Scholar
27. Breslau N, Fenn N, Peterson EL: Early smoking initiation and nicotine dependence in a cohort of young adults. Drug Alcohol Depend 1993; 33:129–137Crossref, Medline, Google Scholar
28. Simmons RG, Burgeson R, Carlton-Ford S, Blyth DA: The impact of cumulative change in early adolescence. Child Dev 1987; 58:1220–1234Google Scholar
29. McCubbin HI, Needle RH, Wilson M: Adolescent health risk behaviors: family stress and adolescent coping as critical factors. Family Relations 1985; 34:51–62Crossref, Google Scholar



