Clinical Computing: A Web-Based Data Management System to Improve Care for Depression in a Multicenter Clinical Trial
In 2001 more than half of all Americans had access to the Internet, and many were using it to seek information about health problems such as depression (1). Researchers have also started to use the Internet to support data collection in multicenter studies (2,3,4,5). In this column we describe a Web-based data management system developed to support a multicenter trial of a disease management program for late-life depression in primary care (Project IMPACT) (6).
In earlier studies, we used paper-based study records to track study recruitment and intervention activities. These records were transmitted to a coordinating center, cleaned, and entered into a database by research assistants. This process consumed a substantial amount of time and resources, and questions about data content often could not be answered in the absence of the staff who had originally generated the data. The clinicians who provided intervention services thought that a computerized tracking and reminder system would better facilitate their clinical work than a paper-based charting system.
Development of a Web-based data management system
For Project IMPACT (6), we developed a Web-based data management system that can be accessed over the Internet on a 24-hour basis by study staff at 18 participating clinics. The system was developed at the University of California, Los Angeles (UCLA) and was tested with the help of study staff at all participating sites. The system was implemented with use of an Apple Power Mac G3 computer running Mac OS X as a server (Apple Computer, Cupertino, Calif.) and was programmed with WebObjects (Apple) and the FrontBase SQL database (FrontBase, Foothill Ranch, Calif.).
To ensure the security and integrity of our data, we used technology similar to that used to protect credit card information in e-commerce applications: all exchanges between a user's browser and the server are two-way encrypted with the secure sockets layer (SSL) protocol to prevent eavesdropping, tampering, or data forgery. SSL protocols use 128-bit cryptography algorithms, such as RC4, which have emerged as standard approaches to high-grade online privacy protection.
As a further safeguard, access to all data on the server is controlled by password protection. Different user profiles allow access to relevant sections of the database. For example, study clinicians can view and edit data on their own patients only. Investigators can see recruitment and intervention data for their study site and de-identified summary data for all study sites for comparison. For additional security of the data, we use only unique study identification numbers to identify study patients on data forms, and we do not transmit patients' names, medical record numbers, or other identifying information over the Internet.
Research applications
The system supports many study-related data management tasks. Local recruiters record their activities on Web-based data entry forms, and the system allows recruiters, project coordinators, and study investigators to monitor recruitment activities in "real time." A total of 1,801 patients are enrolled in the study, and the information system helps investigators track enrollments, disenrollments (with reasons for disenrollments), contact information, and completion of baseline and follow-up assessments. It also tracks laboratory values (hemoglobin A1c) for a subset of patients who are participating in a study of the effects of depression treatment on glycemic control (6). Project coordinators receive reminders about patients who are due for hemoglobin A1c follow-up measurements when they log on to the system.
Clinical applications
The clinical applications are used primarily by clinical specialists in depression, nurses, or clinical psychologists who care for intervention patients at one of the participating study sites (6). These clinicians record data from all initial assessments, follow-up contacts, treatment plans, and relapse-prevention plans during the 12-month intervention period. Acute-phase treatment plans are time limited—up to 12 weeks—to prevent patients from spending excessive time on ineffective treatments.
The Web-based data entry forms are structured, which facilitates the standardization of the intervention model across study sites. The database is programmed to give individual clinicians reminders about patients who have not had initial assessments or follow-up contacts or whose treatment plans have "expired" and may be ineffective. Because this information is available in real time, the system can be used by investigators and clinical supervisors to monitor and support the implementation and standardization of the intervention across participating sites.
Clinical specialists in depression can use the system to compare their caseloads with summary figures for all other depression clinical specialists in the system, to display treatment histories for individual patients (Figure 1), to produce summaries of all their active cases (Figure 2), or to access individual clinical notes, treatment plans, and psychiatric consultation notes. The depression clinical specialists bring copies of such summaries to their weekly supervision meetings with a team psychiatrist and share printed copies of their notes and treatment plans with patients and their primary care providers.
Experience and limitations
The system has been in continuous use since July 1999 and requires limited ongoing database maintenance and end-user support. The coordinating center worked with each site to ensure that study staff had access to the Internet and that they were familiar with the system. In addition to initial group training, most users required some individual training in the use of the system. Frequent users, such as recruiters and depression clinical specialists, quickly learned the system, but infrequent users, such as study psychiatrists, either took longer to learn or preferred to make handwritten consultation notes and have other staff members enter the data for them.
To date, 22 study recruiters and 11 project coordinators have logged more than 11,630 sessions to record recruitment activities, including more than 20,000 initial screenings, 4,264 eligibility interviews, and 1,801 baseline interviews. The 18 depression clinical specialists have logged 9,348 sessions, recording 883 initial clinical assessments, 13,103 in-person and telephone follow-up contacts, and 2,046 treatment plans. These specialists spend about 10 percent of their time on study-related documentation activities, including the use of the Web-based data management system.
The current system has several advantages over older, paper-based methods. Information about recruitment, enrollment, and clinical activities is available to study staff in real time. Data are entered by site-based study staff, which minimizes the possibility of subsequent transcription or data entry errors by staff members who are unfamiliar with the data and also saves valuable time at the end of the study. Simple error-checking routines were programmed into the data collection forms with client-side Java Script to ensure completion of required data fields and to minimize the number of out-of-range values. Data are immediately transferred to the coordinating center, where they are secured and routinely backed up, which minimizes the possibility of data loss.
Clinician users value the search and reporting features of the system and the reminders that facilitate treatment according to the intervention protocol. In an earlier study of a similar intervention program, 73 percent of eligible patients received an initial assessment from a depression clinical specialist (7). In this study, depression clinical specialists receive a reminder that a patient is overdue for an initial assessment if no assessment has been recorded within 30 days of the patient's enrollment. This simple reminder may be partly responsible for the fact that 99 percent of the intervention patients receive initial assessments.
Although the system has been well received, it has several limitations. It is not integrated into existing clinical record systems, which means that some depression clinical specialists have to enter information into the Web-based study system and into their local record systems. Although we had initially envisioned that most study clinicians would enter information directly into the computer during patient contacts, many clinicians find this difficult to do and prefer to complete paper versions of the visit forms and to enter them into the Web-based system later. Some depression clinical specialists find it difficult to capture or obtain certain types of clinical information because of a lack of a designated field in the database.
Future applications
Future applications of Web-based data systems could be programmed to generate patient assignments in randomized controlled trials. A Web-based system that uses streaming video could also be used to standardize training of research staff in multisite trials on assessment instruments and other study procedures. Such a system is currently under development at the UCLA Neuropsychiatric Institute's Academic Information Technology Core.
On the clinical side, patients and their primary care providers could be given access to the Web-based data system. The system could provide patient education tailored to individual needs that could be viewed by patients and their significant others at a convenient time and place. Patients could complete depression assessments either via a study Web site or by using a touch-tone telephone with an interactive voice-response program (8,9). This information would allow treating clinicians to focus their energy on patients whose depression has not sufficiently improved or who are experiencing a relapse.
Other researchers (9,10,11,12) have experimented with Web-based versions of structured psychotherapies. A Web-based application could also facilitate patient-provider communication or communication with peer counselors or other patients (through a chat-group format), appointment scheduling, or prescription refill requests. Finally, it would be useful to explore the option of user-friendly ap-pliances, such as wireless handheld computers, to facilitate data entry during patient encounters.
Acknowledgments
Project IMPACT was developed with funding from the John A. Hartford Foundation and the California HealthCare Foundation.
The authors are affiliated with the Neuropsychiatric Institute of the University of California, Los Angeles. Address correspondence to Dr. Unützer, Center for Health Services Research, UCLA Neuropsychiatric Institute, 10920 Wilshire Boulevard, Suite 300, Los Angeles, California 90024 (e-mail, [email protected]). Joshua Freedman, M.D., is editor of this column.
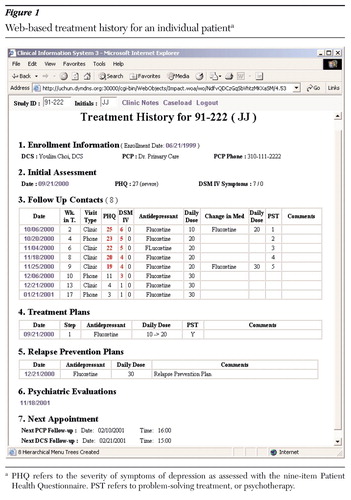
Figure 1. Web-based treatment history for an individual patienta
a PHQ refers to the severity of symptoms of depression as assessed with the nine-item Patient Health QuestionnairePST refers to problem-solving treatment, or psychotherapy.
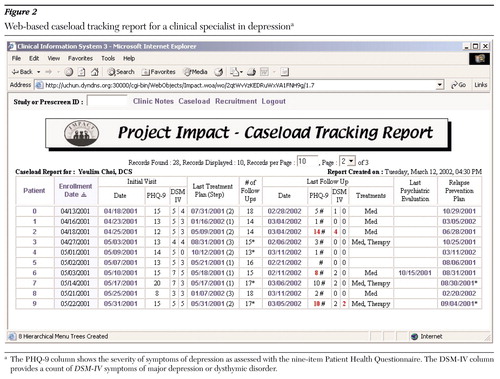
Figure 2. Web-based caseload tracking report for a clinical specialist in depressiona
a The PHQ-9 column shows the severity of symptoms of depression as assessed with the nine-item Patient Health QuestionnaireThe DSM-IV column provides a count of DSM-IV symptoms of major depression or dysthymic disorder.
1. Eng TR: The eHealth Landscape: A Terrain Map of Emerging Information and Communication Technologies in Health and Health Care. Princeton, NJ, Robert Wood Johnson Foundation, 2001Google Scholar
2. Marks R, Bristol H, Conlon M, et al: Enhancing clinical trials on the Internet: lessons from INVEST. Clinical Cardiology 24(11 suppl):V17-V23, 2001Google Scholar
3. Marks RG, Conlon M, Pepine CJ: Paradigm shifts in clinical trials enabled by information technology. Statistics in Medicine 20:2683-2696, 2001Crossref, Medline, Google Scholar
4. Pepine CJ, Handberg-Thurmond E, Marks RG, et al: Rationale and design of the international verapamil SR/trandolapril study (INVEST): an Internet-based randomized trial in coronary artery disease patients with hypertension. Journal of the American College of Cardiology 32:1228-1237, 1998Crossref, Medline, Google Scholar
5. Niland JC, Stahl D, Rouse MS: An Internet-based database system for outcomes research in the National Cancer Center and community settings. Presented at the annual meeting of the American Medical Informatics Association, November 5, 2001Google Scholar
6. Unützer J, Katon W, Williams Jr JW, et al: Improving primary care for depression in late life: the design of a multicenter randomized trial. Medical Care 39:785-799, 2001Crossref, Medline, Google Scholar
7. Rubenstein LV, Jackson-Triche M, Unützer J, et al: Evidence-based care for depression in managed primary care practices. Health Affairs 18:89-105, 1999Crossref, Medline, Google Scholar
8. Greist JH: The computer as clinician assistant: assessment made simple. Psychiatric Services 49:467-472, 1998Link, Google Scholar
9. Greist JH: Treatment for all: the computer as a patient assistant. Psychiatric Services 49:887-889, 1998Link, Google Scholar
10. Selmi PM, Klein MFI, Greist JH, et al: Computer-administered cognitive-behavioral therapy for depression. American Journal of Psychiatry 147:51-56, 1990Link, Google Scholar
11. Osgood-Hynes DJ, Greist JH, Marks IM, et al: Self-administered psychotherapy for depression using a telephone-accessed computer system plus booklets: an open US-UK study. Journal of Clinical Psychiatry 59:358-365, 1998Crossref, Medline, Google Scholar
12. Budman S: Behavioral health care dot-com and beyond: computer-mediated communications in mental health and substance abuse treatment. American Psychologist 55:1290-1300, 2000Crossref, Medline, Google Scholar