Suicide Risk Assessment and Content of VA Health Care Contacts Before Suicide Completion by Veterans in Oregon
Veterans are twice as likely as nonveterans to die by suicide ( 1 ), and each year as many as 5,000 veterans take their own lives ( 2 ). Research has indicated that a considerable proportion of individuals who complete suicide make contact with health care clinicians before death. A review of 40 studies of contact with clinicians before suicide found that approximately 45% of individuals made contact in the month before death with primary care clinicians and 19% made contact with mental health care clinicians ( 3 ). Older individuals more commonly made contact with primary care; an average of 58% of adults over age 55 contacted primary care clinicians in the month before death, and 11% contacted mental health clinicians. As a result, increased attention has been given to the role that clinicians can play in suicide prevention ( 4 , 5 , 6 ).
However, very little is known about the content of health care visits that occur proximal to veterans' suicides and what opportunities exist for intervention. Specifically, among veterans who subsequently complete suicide, almost nothing is known about how often clinicians assess for psychiatric disorders that place veterans at higher risk of suicide, including depression, posttraumatic stress disorder (PTSD), and substance use disorders ( 7 , 8 , 9 , 10 ). Further, it is not known how often high-risk veteran patients endorse thoughts of suicide when clinicians inquire about suicidal ideation or to what extent these patients visit clinicians asking for help or demonstrating emotional distress. Because general medical illness has been shown to be associated with suicide risk ( 1 , 4 , 11 ), it may be that many patients contact their clinicians before suicide as part of routine care for general medical problems.
This retrospective study sought to further our understanding of the clinical care experience of veterans before suicide by describing their health care contacts in the year before their death. Specifically, we linked death certificate data from the Oregon Violent Death Reporting System (OVDRS) to health care data available from the Veterans Integrated Service Network 20 (VISN 20) Data Warehouse to identify all veterans aged 18 and older who completed suicide in Oregon between 2000 and 2005 and who had one or more health care-related contacts with a single Department of Veterans Affairs Medical Center (VAMC) in the 12 months before death. We present demographic, utilization, and diagnostic data for the sample and describe clinicians' documentation of whether they explored for the presence of psychiatric features associated with suicide risk and reasons for each veteran's last contact.
Methods
This study was a retrospective medical record review of veteran decedents identified by county medical examiners as having completed suicide in the state of Oregon between 2000 and 2005. Approvals for this study were obtained from the local VAMC institutional review board (exempt status) and from the Oregon Public Health Division.
Data sources and population
OVDRS provided death certificate data for decedents aged 18 and over who completed suicide in Oregon between 2000 and 2005. OVDRS data included the last four digits of each decedent's Social Security number, name, date of birth, date of death, cause of death, veteran status, sex, race-ethnicity, highest level of education, and marital status. The OVDRS defines suicide death by ICD-10 codes X60–X84, and Y87.0 as the underlying cause of death on death certificates. In a previous nationwide comparison of Vietnam-era veteran death certificates and medical review data, death certificate recording of suicide was 90% sensitive and specific ( 12 ).
We matched OVDRS data to administrative data from the VISN 20 Data Warehouse using the last four digits of the Social Security number, name, and date of birth. The VISN 20 Data Warehouse contains data extracted from the electronic patient record files of regional VA facilities; it is updated monthly, and reliability checks are performed regularly. The VISN 20 Data Warehouse has been used in previous studies of utilization of services and medications ( 13 , 14 ). Veteran status was assigned if the decedent was designated as a veteran by either VISN 20 or OVDRS data. A national comparison between death certificates and the U.S. Census Bureau's Population Survey indicated that the designation of veteran status on death certificates agrees 95% of the time with baseline veteran status ( 15 ). On the basis of utilization data extracted from the VISN 20 Data Warehouse, we identified 114 veterans who had received health care services at any of the programs or clinics belonging to the VAMC system in the 12 months before death. Receipt of services was defined as any contact, including phone, prescription refill, inpatient stay, and outpatient visit. Using medical record review, we then identified the 112 veterans who had one or more phone or in-person contacts with health care personnel characterized by two-way communication between the patient and health care personnel. These did not include phone messages, letters, or requests for prescription refills. This group (N=112) constituted the sample for this study.
We manually reviewed patient medical records for the 112 veterans to determine whether any clinician assessed the veteran for symptoms of depression, a substance use disorder, PTSD, or suicidal ideation. These psychiatric features were chosen on the basis of evidence of association with suicide risk ( 7 , 8 , 9 , 10 ). Assessment was defined as any clinician-documented exploration of these risk factors, ranging from use of formal, templated screening tools to narrative in progress notes. Although screening tools were in use during the time frame of this study for depression, substance use, and PTSD, formal screening tools for suicidal ideation were not. For each of these risk factors, we recorded the assessment (if any) most proximal to the date of death. We also report whether this assessment occurred within 30 days before death and whether it occurred during the contact most proximal to the date of death (last contact).
When the patient record documented current suicidal ideation, we also recorded whether the clinician documented assessment of additional suicide risk and protective factors ( 16 ), either that day or within 30 days. This included discussion of previous attempts; determination of passive versus active suicidal ideation; documentation of hopelessness, impulsivity, recent losses or stressors, access to lethal means, and social support; and arrangement for clinical follow-up. Passive suicidal ideation was defined as having thoughts about suicide or about being better off dead but no specific ideation about methods or intent to harm oneself. Active suicidal ideation included expressing a desire to die, identifying a possible method, or specific planning or intent.
For each veteran's last contact, we recorded clinician-documented reasons for the contact (either a routine follow-up or a patient-initiated contact for a new or exacerbated medical concern) and whether the clinician noted any emotional distress. Last contacts were considered to be follow-ups if the patient and clinician discussed conditions previously known to the clinician and if the visit was not clearly initiated by the patient's concern over exacerbation of a known problem. Emotional distress was indicated by documentation of distress over a particular general medical or mental health concern (diagnoses were not sufficient) or difficulty coping with stressful life events. We also recorded whether the patient had received non-VA health care during the year before death, as indicated by outside medical records embedded in the VA electronic record or VA clinician notation in progress notes.
After initial testing and subsequent refinement of a medical record review checklist and development of a codebook, two trained reviewers (LMD and MCC) reviewed each patient's chart. When there were disagreements, a third reviewer (SKD or KCD) arbitrated.
Demographic data were extracted from OVDRS data, and ICD-9-CM diagnostic and utilization data for the year before death were extracted from the VISN 20 Data Warehouse.
Setting
The VAMC is a general medical and surgical teaching facility with five primary care clinics, which served approximately 42,000 veterans enrolled during the study period (2000–2005). Two primary care clinics located in a metropolitan area served approximately 28,000 patients during this period. Clinics were also located in another medium-sized city (serving 6,000 patients) and two rural locations (serving 1,000 and 4,000, respectively). Since 1998, all inpatient and outpatient progress notes, prescription refills, and phone contacts have been maintained in a systemwide electronic patient record system.
Analysis
Basic frequencies and other descriptive statistics were used to describe the sample, health care utilization, and content of clinician assessments. Results are presented for the year before death, the 30 days before death, and the last contact before death. All analyses were conducted using SPSS, version 16 or 17.
Results
Sample characteristics
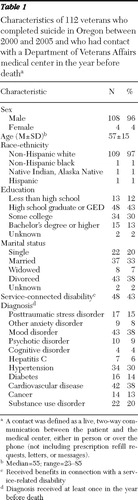
Table 1 presents selected characteristics of the 112 veterans in the sample. Ages ranged from 23 to 85 years, with a mean age of 57. Of note, common diagnoses were mood disorders (38%) and cardiovascular disease (38%). Medical records indicated that almost half of the veterans (N=53, 47%) had accessed health care outside the VA system in the year before death.
 |
VAMC care experiences in the 12 months before death
In the year before death, almost half of the veterans (N=54, 48%) had at least one mental health contact at the VAMC, including nine (8%) who had at least one substance abuse treatment program contact. Seventy-one (63%) had at least one primary care contact, and 62 (55%) had at least one emergency department contact. Table 2 presents data on the number of veterans assessed for selected risk factors during the 12 months before death. All 11 of the veterans who endorsed suicidal ideation received further assessment of suicide risk and protective factors within 30 days of the endorsement, including discussion of previous attempts, passive versus active suicidal ideation, hopelessness, impulsivity, recent losses or stressors, access to lethal means, and social support and arrangement for clinical follow-up. For four of the 11 veterans, active suicidal ideation was documented.
 |
VAMC care experiences in the 30 days before death
In the 30 days before death, 61 (54%) of the veterans had at least one VAMC health care contact. Twenty-three (21%) had at least one mental health contact, including five (4%) who had at least one substance abuse program contact. Seventeen (15%) had at least one primary care contact, and 15 (13%) had at least one emergency department contact. Table 2 presents data on the number of veterans assessed for selected risk factors during the 30 days before death. All six who endorsed suicidal ideation during this period received further suicide risk assessment within 30 days of the endorsement. Of those, three endorsed active suicidal ideation.
VAMC care experiences during the last contact
The median number of days between patients' last VAMC contact and the date of death was 42 (range=0–358). Twenty-six (23%) of the 112 veterans received care in a mental health setting during their final contact, which includes four (4%) who were seen in a substance abuse treatment program. Twenty-two (20%) of the veterans received care in primary care, and 13 (12%) were seen in the emergency department. The remaining 51 (46%) had their last contact with other specialty services. Eighteen (16%) were assessed for suicidal ideation, but almost three-quarters of those who were assessed (N=13, 72%) denied suicidal ideation at that time ( Table 3 ). All five who endorsed suicidal ideation received further suicide risk assessment within 30 days. Of those, two endorsed active suicidal ideation.
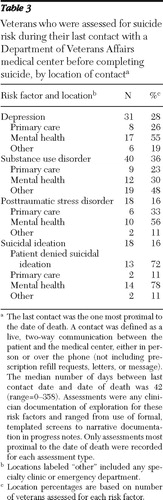 |
Of the 26 veterans whose final contacts were in a mental health setting, 20 (77%) were assessed on that day for depression, a substance use disorder, or PTSD, and 14 (54%) were assessed for suicidal ideation. Of the 22 veterans whose final contacts were with primary care, ten (45%) were assessed for depression, a substance use disorder, or PTSD, and two (9%) were assessed for suicidal ideation on that day. Of the 64 veterans whose final contacts were with emergency or other specialty services, 23 (36%) were assessed on that day for depression, a substance use disorder, or PTSD, and two (3%) were assessed for suicidal ideation. Thirty-six (32%) of the 112 veterans' last contacts were patient initiated for a new or exacerbated medical concern, and 76 (68%) were follow-ups for an ongoing medical concern. Eight (7%) were seen in a group educational or treatment setting. During 41 (37%) of the last contacts, clinicians noted that the patient was experiencing emotional distress.
Discussion
Of the 112 veterans aged 18 and over who completed suicide in Oregon between 2000 and 2005 and who had contact with the VAMC in the year before death, 63% received primary health care and almost half received mental health care during the year. Just over half of the veterans received care in the 30 days before death, with 21% receiving mental health care and 15% receiving primary care. Forty-one percent of these patients were assessed for suicidal ideation during the year before death, and 16% were assessed during their last contact. However, most of these patients (68%) received care under fairly routine circumstances at their last contact. About three-quarters of patients who were asked about thoughts of suicide denied such thoughts; however, when patients endorsed suicidal ideation, clinicians consistently documented follow-up for it.
More than half of the patients who received care in a mental health setting at their last contact were assessed for suicidal ideation, whereas only 9% of those whose last contact was in a primary care setting were assessed for suicidal ideation. These results are consistent with a study of British suicide victims, which found that only two of 61 patients who had been seen by their general practitioner were assessed for suicide risk during their final appointment ( 17 ). However, in the study reported here, some veterans had been assessed for thoughts of suicide during the past year; clinicians may not have addressed suicide in the last contact if the veteran had previously responded negatively to questions about suicidal ideation. Indeed, nine of the 26 veterans whose last contact was with mental health had been previously assessed for thoughts of suicide during the past year, whereas only two of the 22 whose last contact was with primary care had been previously assessed for thoughts of suicide during the year.
Although it is reasonable to expect that mental health clinicians would be more likely than other clinicians to discuss mental health concerns with patients, our results suggest that primary care clinicians have more opportunities to talk with patients about suicide, given the larger number of veterans seen in primary care. However, competing demands on time and other barriers, such as comfort level with the topic, may make it challenging for providers to discuss suicide risk with their patients ( 4 ). Our results also suggest that there are often few clinical indicators to trigger discussion of suicide risk with patients.
Indeed, recognizing when to ask patients about suicide is extraordinarily complex. Our finding that nearly two-thirds of the veterans' last contacts were part of planned follow-up care suggests that most patients who visit their care clinician in the year before completing suicide see their clinicians under relatively routine circumstances. Further, in only about one-third of the patients' last visits did clinicians note emotional distress. These circumstances underscore the difficulty of distinguishing patients at risk from those participating in routine care.
Unfortunately, we also found little evidence to suggest that inquiring about suicide will successfully identify the veterans most at risk of suicide. Three-quarters of those who were asked about thoughts of suicide in the year before death denied such thoughts. Fear of stigma or appearing weak might prevent many veterans from disclosing thoughts of suicide, especially among those most in need of mental health services ( 18 , 19 ). Alternatively, some of these veterans may not have had suicidal thoughts at the time of clinician assessment. This finding suggests that screening for suicidal ideation may have limited value for identifying such thoughts. Recent reviews of suicide prevention strategies have noted the lack of evidence to support routine screening for identifying and preventing suicide for most patients ( 6 , 20 , 21 ), and our findings further emphasize the need for more knowledge of how to best facilitate patient-clinician communication about suicidal thoughts.
Several limitations should be considered in interpreting these results. Most important, data gathered through manual record review are limited by what a clinician documents for each visit. If the clinician received a negative response to inquiries about depression or suicide, for example, he or she might not have noted this in the chart. We did not rate clinicians' attention to other potentially important factors, such as functional decline or increased social withdrawal, because we have found these constructs too difficult to code reliably in medical record review studies. Another limitation is that we reviewed suicides by veterans who had been seen at only a single VAMC. Our results do not include those who may have received care in other VA facilities or the three-quarters of veterans who do not receive VA health care ( 22 ). However, a previous study of veterans who completed suicide showed few demographic differences between veterans who received VA health care and those who did not (Basham C, Denneson LM, Millet L, et al., unpublished manuscript, 2009). Furthermore, the VA health system has considerably enhanced suicide prevention efforts since 2005, including provision of new staff education programs, implementation of formal screening for suicidal ideation, and emphasis on conducting suicide risk assessment for at-risk patients ( 23 ). Our results should be interpreted as reflective of the time frame during which the data were collected. However, we note that because many veterans in our study denied suicidal ideation, implementation of formal screening processes would likely have had limited impact.
Conclusions
This study highlights the complexity of addressing suicidal ideation and associated risk factors in health care settings. Most of the veterans who completed suicide were seen for routine medical care and did not have apparent signs of emotional distress at their last clinical contact. Thus there was limited obvious indication for further exploration of suicide risk factors or suicidal ideation. Further, a number of veterans who went on to complete suicide either did not have thoughts of suicide at the time of their last contact with clinicians or denied such thoughts, even when questioned by clinicians. Effective health care-based suicide prevention strategies would benefit from additional research to identify better ways to enhance communication of suicidal thoughts when they are present.
Acknowledgments and disclosures
This article is based on work supported in part by the VA, the Veterans Health Administration, and VA Health Services Research and Development Service Project DHI-08-096. The views expressed are those of the authors and do not necessarily reflect the position or policy of the VA or the U.S. government.
The authors report no competing interests.
1. Kaplan MS, Huguet N, McFarland BH, et al: Suicide among male veterans: a prospective population-based study. Journal of Epidemiology and Community Health 61:619–624, 2007Google Scholar
2. Healthcare Inspection: Implementing VHA's Mental Health Strategic Plan Initiatives for Suicide Prevention. Washington, DC, US Department of Veterans Affairs, Office of the Inspector General, May 2007. Available at va.gov/oig/54/reports/vaoig-06-03706-126.pdf Google Scholar
3. Luoma JB, Martin CE, Pearson JL: Contact with mental health and primary care providers before suicide: a review of the evidence. American Journal of Psychiatry 159:909–916, 2002Google Scholar
4. Schulberg HC, Bruce ML, Lee PW, et al: Preventing suicide in primary care patients: the primary care physician's role. General Hospital Psychiatry 26:337–345, 2004Google Scholar
5. Valenstein M, Kim HM, Ganoczy D, et al: Higher-risk periods for suicide among VA patients receiving depression treatment: prioritizing suicide prevention efforts. Journal of Affective Disorders 112:50–58, 2009Google Scholar
6. Mann JJ, Apter A, Bertolote J, et al: Suicide prevention strategies: a systematic review. JAMA 294:2064–2074, 2005Google Scholar
7. Simon GE, VonKorff M: Suicide mortality among patients treated for depression in an insured population. American Journal of Epidemiology 147:155–160, 1998Google Scholar
8. Zivin K, Kim HM, McCarthy JF, et al: Suicide mortality among individuals receiving treatment for depression in the Veterans Affairs health system: associations with patient and treatment setting characteristics. American Journal of Public Health 97: 2193–2198, 2007Google Scholar
9. Lehmann L, McCormick RA, McCracken L: Suicidal behavior among patients in the VA health care system. Psychiatric Services 46:1069–1071, 1995Google Scholar
10. Waller SJ, Lyons JS, Costantini-Ferrando MF: Impact of comorbid affective and alcohol use disorders on suicidal ideation and attempts. Journal of Clinical Psychology 55:585–595, 1999Google Scholar
11. Goodwin RD, Marusic A, Hoven CW: Suicide attempts in the United States: the role of physical illness. Social Science and Medicine 56:1783–1788, 2003Google Scholar
12. Moyer LA, Boyle CA, Pollock DA: Validity of death certificates for injury-related causes of death. American Journal of Epidemiology 130:1024–1032, 1989Google Scholar
13. Dobscha S, Corson K, Hickam D, et al: Depression decision support in primary care: a cluster randomized trial. Annals of Internal Medicine 145:477–487, 2006Google Scholar
14. Dobscha SK, Anderson TA, Hoffman WF, et al: Strategies to decrease costs of prescribing selective serotonin reuptake inhibitors at a VA Medical Center. Psychiatric Services 54:195–200, 2003Google Scholar
15. Sorlie PD, Rogot E, Johnson NJ: Validity of demographic characteristics on the death certificate. Epidemiology 3:181–184, 1992Google Scholar
16. Martin J, Ghahramanlou-Holloway M, Lou K, et al: A comparative review of US military and civilian suicide behavior: implications for OEF/OIF suicide prevention efforts. Journal of Mental Health and Counseling 31:101–118, 2009Google Scholar
17. Appleby L, Amos T, Doyle U, et al: General practitioners and young suicides: a preventive role for primary care. British Journal of Psychiatry 168:330–333, 1996Google Scholar
18. Hoge CW, Castro CA, Messer SC, et al: Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine 351:13–22, 2004Google Scholar
19. Stecker T, Fortney JC, Hamilton F, et al: An assessment of beliefs about mental health care among veterans who served in Iraq. Psychiatric Services 58:1358–1361, 2007Google Scholar
20. Shekelle P, Bagley S, Munjas B: Strategies for Suicide Prevention in Veterans. Washington, DC, US Department of Veterans Affairs, Health Services Research and Development Service, 2009Google Scholar
21. Gaynes BN, West SL, Ford CA, et al: Screening for suicide risk in adults: a summary of the evidence for the US Preventive Services Task Force. Annals of Internal Medicine 140:822–835, 2004Google Scholar
22. 2001 National Survey of Veterans. Washington, DC, Department of Veterans Affairs, 2001. Available at va.gov/vetdata/surveysandstudies/final_report.asp Google Scholar
23. The Comprehensive VHA Mental Health Strategic Plan. Washington, DC, US Department of Veterans Affairs, May 2005Google Scholar



