Comparative Prevalence of Psychotropic Medications Among Youths Enrolled in the SCHIP and Privately Insured Youths
Abstract
The one-year prevalence of use of psychotropic medications among youths enrolled in a Mid-Atlantic State Children's Insurance Program (SCHIP) in 1999 or 2000 was compared with the 1998-2000 prevalence findings for youths enrolled in four large multistate private medical insurance programs. Prevalence was significantly higher among youths enrolled in the SCHIP than among those with private insurance in all eight medication group comparisons. Unlike private insurance, the surveyed state SCHIP program did not require a copayment or have a restrictive formulary. These administrative differences may partly explain the comparatively higher rate of psychotropic use under the SCHIP.
In large data-based studies of the prevalence of use of psychotropic medications among youths that compared results in relation to type of medical insurance, it has been apparent that youths who are covered by Medicaid have higher rates of use than youths with private insurance (1). The higher rates may be explained by the fact that youths enrolled in Medicaid have, as a group, a greater degree of impairment (2).
Functioning administratively within the Medicaid insurance program in a Mid-Atlantic state, the State Children's Insurance Program (SCHIP) is an eligibility category whose enrollees are most comparable to privately insured individuals. Studies of children enrolled in the SCHIP indicate that 80 to 91 percent of these children live with at least one employed adult, rates that are not much lower than the rate of 97 percent seen among privately insured children (3). However, race, ethnicity, and the family characteristics of SCHIP enrollees vary from state to state and can be quite different from those of persons with private insurance. For example, whereas 13 percent of privately insured youths live in single-parent households, the rate for SCHIP youths ranges from 18 to 51 percent (4).
The preliminary investigation reported here focused on the prevalence of use of psychotropic medications among SCHIP-enrolled youths in a midsized Mid-Atlantic state compared with the rate among age-matched, privately insured youths recorded from four large multistate data sets. A single-state comparison of treatment patterns of youths with different types of insurance would be optimal, and one such comparison is presented here.
Methods
The SCHIP data came from cross-sectional analyses of administrative and pharmacy claims over two one-year periods from one state for the years 1999 and 2000. This research was approved by the institutional review boards of the University of Maryland, Baltimore, and the State Department of Health and Mental Hygiene. The multistate data sets containing cross-sectional, annually recorded information about privately insured youths included MarketScan (5,6), Express Scripts (7), health plans affiliated with the United Health Group (8), and an unidentified large multistate data set (9). The prevalence comparisons included rates either for the same year or for two years that were one year apart. The private insurance and SCHIP data were also matched for age strata and medication class. The analyses covered the prevalence of use of stimulants, selective serotonin reuptake inhibitors, and the category "any psychotropic medication." Annual prevalence was calculated as the number of youths who had one or more psychotropic drug dispensings per 100 enrolled youths. Confidence intervals are reported for the prevalence data.
Results
The 1999 and 2000 data on the one-year prevalence of use of psychotropic medication for Mid-Atlantic state youths in the SCHIP eligibility category and privately insured youths in four multistate data sets are compared in Table 1. Even though the prevalence of use among Mid-Atlantic SCHIP enrollees was sizably lower than that in the other three major Medicaid eligibility categories in that state (10), it was still consistently higher in all eight comparisons (range, 19 to 60 percent) with privately insured youths residing in numerous states (5,6,7,8,9).
The 1999 Express Scripts multistate data on the prevalence of stimulant treatment among privately insured youths aged five to 14 years was reported by state (7). Its annual prevalence of stimulant treatment in the surveyed Mid-Atlantic state was 4 percent (95 percent confidence interval [CI]=3.6 to 4.4), whereas the prevalence for that state's age-matched SCHIP enrollees was 7 percent (CI=6.7 to 7.4).
Discussion
The major finding of this comparative analysis was that youths who were enrolled in the SCHIP in this Mid-Atlantic state had a consistent and substantially higher prevalence of use of psychotropic medications than age-matched youths enrolled in four multistate private insurance programs during the years 1998 to 2000. This difference was also observed for the one state comparison between youths covered by the SCHIP and those with private insurance.
There are several possible explanations for this unexpected finding. Administrative factors that may have influenced the comparative analysis include the fact that health practitioners in the Mid-Atlantic SCHIP are paid on a fee-for-service basis arranged through managed care organizations, whereas those reimbursed by private insurers are funded by a mix of capitated and fee-for-service arrangements. The influence of the payment difference on the results of this analysis is not known. Several additional financial and prescription policy differences between the SCHIP in this state and multistate private insurance carriers are described below.
Dispensing of psychotropic medications under the SCHIP in 1999 and 2000 in the Mid-Atlantic state did not require out-of-pocket payments. By contrast, private insurance copayments were reported to range up to $60 for a brand-name drug and $30 for a generic drug (7,8). Copayment policies have consistently been shown to decrease the number of dispensings.
In 1999 and 2000, Mid-Atlantic SCHIP insurance did not have formulary restrictions on psychotropic medications for youths. By contrast, formulary restrictions were in place in more than 75 percent of private insurance plans in 2000. Enrollees of private insurance programs—for example, the United Health Group—have been commonly charged $25 or more for drugs that are not on a preferred list (8).
Other factors that may have differentially influenced the findings include racial disparities. Systematic studies that have evaluated the prevalence of use of psychotropic medications by race or ethnicity have all found that youths from racial or ethnic minority groups have approximately half the rate of use of white youths (1,10). As in other U.S. states (4,5), youths from minority groups are overrepresented (62 percent) in the Mid-Atlantic SCHIP population (10). In national surveys of parents, white youths have represented 70 to 75 percent of the population (1). One would therefore expect the prevalence of use of psychotropic medications among SCHIP enrollees to be distinctly lower than that among individuals with private insurance. The fact that the opposite is true suggests that the rate among those with private insurance is low.
Surveys of parents suggest that 3 to 11 percent of their offspring who are SCHIP enrollees have fair to poor health. This rate is approximately twice as high as that in the general population (4). Presumably, increased impairment serves to increase the prevalence of use of medication among SCHIP enrollees.
Restricted access to care would be expected to have a greater impact on families with low incomes and thereby differentially reduce the prevalence of use of psychotropic medications by these families. Given the reverse effect observed in the analysis reported here, access to care is unlikely to explain the results.
Among 1999 United Health Group enrollees, 25 percent of the youths were below the age of five years (8), whereas 53.6 percent of Mid-Atlantic SCHIP enrollees were in that age group (10). Preschool children have a lower rate of use of psychotropic medication. Consequently, the overrepresentation of preschoolers in the SCHIP population would be expected to lower the overall prevalence.
The comparisons presented here are limited in that the study's SCHIP data come from only one U.S. state and the private insurance data from four different multistate data sets. Conclusions are more reliable when comparative medication rates are gathered from the same geographic region. Second, some sociodemographic information was missing in two of the private insurance data sets (5,9).
Conclusions
This analysis showed that youths enrolled in the SCHIP in a mid-sized U.S. state in 1999-2000 had a consistent and substantially greater prevalence of use of psychotropic medications than age-matched youths with private insurance in multiple states in the period 1998 to 2000. The expected positive moderator variable effect of impairment on the prevalence of psychotropic use among SCHIP enrollees appears to be more than offset by the negative moderator effects of age and race or ethnicity. It is likely that this disparity in prevalence is largely the result of the absence of a restrictive formulary and of the requirement for copayments under the SCHIP. Such a hypothesis merits further research.
Dr. Safer is affiliated with the departments of psychiatry and pediatrics at Johns Hopkins University School of Medicine in Baltimore. Dr. Zito is with the School of Pharmacy and the School of Medicine at the University of Maryland in Baltimore and Mr. Gardner is with the School of Pharmacy. Send correspondence to Dr. Safer at 6 Hadley Square North, Baltimore, Maryland 21218 (e-mail, [email protected]).
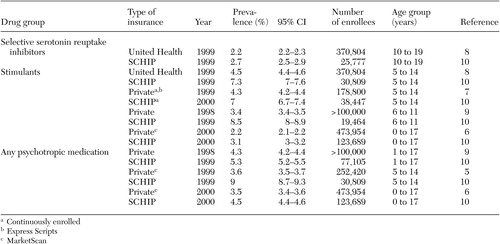 |
Table 1. Prevalence of use of psychotropic medications among youths enrolled in a Mid-Atlantic State Children's Insurance Program (SCHIP) and youths with private insurance in various studies
1. Olfson M, Marcus SC, Weissman MM, et al: National trends in the use of psychotropic medications by children. Journal of the American Academy of Child and Adolescent Psychiatry 41:514–521, 2002Crossref, Medline, Google Scholar
2. Shatin D, Levin R, Ireys HT, et al: Health care utilization by children with chronic illnesses: a comparison of Medicaid and employer-insured managed care. Pediatrics 102:e44, 1998Google Scholar
3. Byck GR: A comparison of the socioeconomic and health status characteristics of uninsured, State Children's Health Insurance program-eligible children in the United States with those of other groups of insured children: implication for policy. Pediatrics 106:14–21, 2000Crossref, Medline, Google Scholar
4. Shone LP, Dick AW, Brach C, et al: The role of race and ethnicity in the State Children's Health Insurance Program (SCHIP) in four states. Pediatrics 112:e521, 2003Google Scholar
5. Martin A, Sherwin T, Stubbe D, et al: Use of psychotropic drugs by Medicaid-insured and privately insured children. Psychiatric Services 53:1508, 2002Link, Google Scholar
6. Martin A, Leslie D: Trends in psychotropic medication costs for children and adolescents, 1997–2000. Archives of Pediatrics and Adolescent Medicine 157:997–1004, 2003Crossref, Medline, Google Scholar
7. Cox ER, Motheral BR, Henderson RR, et al: Geographic variation in the prevalence of stimulant medication use among children 5–14 years old: results from a commercially insured US sample. Pediatrics 111:237–243, 2003Crossref, Medline, Google Scholar
8. Shatin D, Drinkard CR: Ambulatory use of psychotropics by employer-insured children and adolescents in a national managed care organization. Ambulatory Pediatrics 2:111–119, 2002Crossref, Medline, Google Scholar
9. Stein BD, Sturm R, Kapur K, et al: Psychotropic medication costs among youths with private insurance in 1998. Psychiatric Services 52:1152, 2001Link, Google Scholar
10. Zito JM, Safer DJ, Zuckerman IH, et al: The Influence of Medicaid Eligibility Categories and Race on Psychotropic Medication Prevalence in Youths. Presented at the annual meeting of the New Clinical Drug Evaluation Unit, Boca Raton, Fla, June 10–13, 2002Google Scholar



