Adverse Childhood Experiences, Alcoholic Parents, and Later Risk of Alcoholism and Depression
Abstract
OBJECTIVE: The study examined how growing up with alcoholic parents and having adverse childhood experiences are related to the risk of alcoholism and depression in adulthood. METHODS: In this retrospective cohort study, 9,346 adults who visited a primary care clinic of a large health maintenance organization completed a survey about nine adverse childhood experiences: experiencing childhood emotional, physical, and sexual abuse; witnessing domestic violence; parental separation or divorce; and growing up with drug-abusing, mentally ill, suicidal, or criminal household members. The associations between parental alcohol abuse, the adverse experiences, and alcoholism and depression in adulthood were assessed by logistic regression analyses. RESULTS: The risk of having had all nine of the adverse childhood experiences was significantly greater among the 20 percent of respondents who reported parental alcohol abuse. The number of adverse experiences had a graded relationship to alcoholism and depression in adulthood, independent of parental alcohol abuse. The prevalence of alcoholism was higher among persons who reported parental alcohol abuse, no matter how many adverse experiences they reported. The association between parental alcohol abuse and depression was accounted for by the higher risk of having adverse childhood experiences in alcoholic families. CONCLUSIONS: Children in alcoholic households are more likely to have adverse experiences. The risk of alcoholism and depression in adulthood increases as the number of reported adverse experiences increases regardless of parental alcohol abuse. Depression among adult children of alcoholics appears to be largely, if not solely, due to the greater likelihood of having had adverse childhood experiences in a home with alcohol-abusing parents.
An estimated 25 percent of U.S. children are exposed to alcohol abuse or dependence in the family (1). In the 1980s about 21 million adults in the United States grew up with an alcoholic parent (2). As early as 1977, a lay movement to address this issue formally began when the first meeting of Adult Children of Alcoholics was convened to address the health and social problems of this population (3,4). Although self-help groups and publications subsequently flourished (5), scientific investigation of the health and mental health problems of adult children of alcoholics has not kept pace with the development of lay recovery programs and literature (6).
Children living in families with alcohol-abusing parents are more likely than other children to have an unpredictable home life and to carry a burden of secrecy as a result of their attempts to hide the alcohol abuse from others (7,8). These children also have an increased risk of a variety of other adverse childhood experiences, including being abused or neglected, witnessing domestic violence, and being exposed to drug-abusing, mentally ill, suicidal, or criminal household members (9,10,11,12,13,14,15,16,17,18,19,20).
The risk of alcoholism, psychopathology, and other medical and social problems has been reported to be greater among adult children of alcoholics than among other adults (6,21,22,23,24,25). However, little epidemiologic research has quantified the burden of the wide variety of adverse childhood experiences that are more common in alcoholic families and, in turn, the effect of this burden on the risk of alcoholism and depression among adult children of alcoholics.
To address these questions, we used data from more than 9,300 adults in a primary care setting who participated in the adverse childhood experiences study. First, we examined the association between growing up with one or more alcohol-abusing parents and nine adverse childhood experiences. Because previous research has largely ignored the co-occurrence of alcohol abuse in both parents (20), we describe these associations according to whether the mother, the father, or both were alcohol abusers. Because the occurrence of alcoholism and depression may be influenced by both genetic predispositions (26,27,28,29,30,31) and environmental factors (3,4,7,8,9,10,11,12,13,14,15,16,17,18,19,20), we assessed how adverse childhood experiences influenced the risk of alcoholism and depression among persons with and without a history of parental alcohol abuse.
Methods
Setting
The adverse childhood experiences study was based at Kaiser Permanente's San Diego Health Appraisal Clinic, where more than 50,000 adults receive standardized examinations annually. The health appraisals used at the clinic include completion of a standardized medical questionnaire, a physical examination, and review of laboratory results with the patient. All enrollees of the Kaiser Health Plan in San Diego are given literature about this free service. Most members are self-referred, and health care providers refer about 20 percent of the clinic's patients. A recent review of membership and utilization records among Kaiser members in San Diego who were continuously enrolled between 1992 and 1995 showed that 81 percent of those 25 years of age or older had been evaluated in the Health Appraisal Clinic during this four-year interval.
Procedures
The data reported here are from a retrospective cohort analysis of data from the larger study; the methods of the larger study have been reported in detail elsewhere (9,10). The study was approved by the institutional review boards of the Southern California Permanente Medical Group (Kaiser Permanente), the Emory University School of Medicine, and the Office of Protection from Research Risks of the National Institutes of Health.
A total of 13,494 Kaiser Health Plan members who completed standardized medical evaluations at the Health Appraisal Clinic between August 1995 and March 1996 were mailed the study questionnaire, which included questions about childhood abuse and exposure to forms of household dysfunction while growing up. Those who did not respond to the first mailing received a second mailing. The response rate for the survey was 70.5 percent (9,508 members).
We found no important differences between respondents and nonrespondents in health risk behaviors, such as smoking, obesity, and substance abuse, or in history of disease, such as diabetes, hypertension, chronic lung disease, cardiovascular disease, and cancer. Nonrespondents tended to be somewhat younger and to be from racial or ethnic minority groups. Furthermore, after adjustment for differences in age and race, the magnitude of the relationships between a history of sexual abuse and health behaviors and outcomes was nearly identical for respondents and for nonrespondents. Thus we found no evidence that response bias affected the direction or strength of our estimates of the association between a history of sexual abuse and behavioral and health outcomes (32).
We excluded 51 respondents with missing information about race, 34 with missing educational data, and 77 with incomplete information about parental alcohol abuse. The final study cohort of 9,346 included 98 percent of the respondents.
Measures
Parental alcohol abuse. Questions about exposure to parental alcohol abuse during childhood were adapted from the supplement to the 1988 National Health Interview Survey conducted by the National Institute for Alcohol Abuse and Alcoholism (NIAAA) (33). The specific question was "During your first 18 years of life, did you live with anyone who was a problem drinker or alcoholic?" Those who responded affirmatively were asked to check boxes from a list to indicate the identity of the alcohol abuser or abusers. Persons whose father, mother, or both were alcohol abusers were defined as adult children of alcoholics.
Adverse childhood experiences. Questions about adverse childhood experiences asked specifically about the respondent's first 18 years of life. The experiences were verbal abuse, physical abuse, sexual abuse, having a battered mother, parental separation or divorce, and four types of household dysfunction—exposure in the household to drug abuse, mental illness, suicide, or criminal behavior. Questions about verbal and physical abuse and about having a battered mother were adapted from the Conflict Tactics Scale (CTS) (34), for which the five possible responses were never, once or twice, sometimes, often, or very often. Questions about contact sexual abuse were adapted from Wyatt (35). More information about the wording of specific questions for the nine adverse childhood experiences can be obtained from the authors or from previous publications of the adverse childhood experiences study (9,10).
For each respondent we summed the number of adverse childhood experiences to create an "ACE score," which ranged from 0 to 9. The ACE score has been shown to have a robust and graded relationship to unintended pregnancies (36), sexually transmitted diseases (37), numerous health risk factors such as smoking (10), and many of the leading causes of death during adult life (9).
Personal alcoholism and depression. A personal history of alcoholism was defined as an affirmative response to the screening question used in the NIAAA supplement to the 1988 National Health Interview Survey (32), "Have you ever considered yourself to be an alcoholic?"
We used a screening instrument for depressive disorders—major depression and dysthymia—that was developed for the Medical Outcomes Study (38,39). This instrument used data from primary care and mental health subsamples of the Los Angeles Epidemiologic Catchment Area survey (40) and the Psychiatric Screening Questionnaires for Primary Care Patients (41).
The screening instrument includes two questions from the Diagnostic Interview Schedule (DIS) (42): "In the past year, have you had two weeks or more during which you felt sad, blue, or depressed, or lost pleasure in things that you usually cared about or enjoyed?" and "Have you had two years or more in your life when you felt depressed or sad most days, even if you felt okay sometimes?" Respondents who answered yes were asked, "Have you felt depressed or sad much of the time in the past year?"
The instrument also included six questions from the Center for Epidemiologic Studies Depression Scale (CES-D) (43). The CES-D items ask the respondent how often in the past week the following statements were true: "I felt depressed." "My sleep was restless." "I enjoyed life." "I had crying spells." "I felt sad." "I felt that people disliked me." The response scale for these questions was less than one day, one or two days, three or four days, and five to seven days.
The prediction equation developed for this screening tool uses responses to the questions from the DIS and the CES-D; we used a cutoff score of .009 to define a lifetime history of depression (39).
To assess recent problems with depressed affect, we also assessed the relationship of parental alcoholism and adverse childhood experiences to the first question from the DIS.
Statistical analysis
Persons who gave incomplete information about an adverse childhood experience were considered not to have had that experience. This approach would likely have resulted in conservative estimates of the relationship between adverse childhood experiences and health outcomes, because some of those who had had the experience would have been misclassified as not having had it; this type of misclassification would have biased our results toward the null hypothesis (44). However, to assess this potential effect, we repeated our analyses after excluding all respondents with missing information on any of the adverse childhood experiences. The results of this analysis did not differ substantially from the results we report here.
We calculated the adjusted odds ratios and 95 percent confidence intervals for the associations between parental alcohol abuse and each of the nine adverse childhood experiences by using logistic regression. Then we calculated the adjusted odds ratios for the relationships between the experiences and a personal history of alcoholism or depression. Next, we assessed the relationship of the ACE score to these two disorders using five dichotomous variables (ACE scores of 0, 1, 2, 3, or 4 or more); having had no adverse childhood experiences was used as the referent. To test for a trend, we entered the ACE score as an ordinal variable. We then assessed the relationships between parental alcohol abuse and the risk of alcoholism and depression during adulthood with and without control for the ACE score. We included age, sex, race, and education as covariates in all models. Finally, we assessed the prevalence of alcoholism and depression while we controlled simultaneously for the ACE score and for a history of parental alcohol abuse.
Results
The mean±SD age of respondents was 56.6±15.6 years (range, 19 to 94 years). Fifty-four percent (N=5,004) were women, and 79 percent (N=7,380) were white. Forty-two percent (N=3,930) were college graduates, and 7 percent (N=633) had not graduated from high school.
Parental alcohol abuse was reported by 20.3 percent of respondents (N=1,894): mother only (2.3 percent or 213 respondents), father only (15.2 percent or 1,417), and both parents (2.8 percent or 264). The prevalence of parental alcohol abuse declined with the age of the respondent and was higher among women (22.8 percent compared with 17.4 percent).
As Table 1 shows, in contrast with respondents who reported no history of parental alcohol abuse, those who had grown up with at least one alcohol-abusing parent were two or three times as likely to report childhood histories of emotional abuse, physical abuse, sexual abuse, and parental separation or divorce. Respondents who reported a history of parental alcohol abuse were two to five times as likely to have lived during childhood with household members who used illicit drugs, had mental illnesses, attempted suicide, or were criminals (p<.001 for all associations). Respondents who reported parental alcohol abuse were three to eight times as likely to have had a battered mother as those with no history of parental alcohol abuse.
As shown in Table 2, respondents with no history of parental alcohol abuse were less likely to report any of the nine adverse childhood experiences. Among respondents without a parental history of alcohol abuse, 47 percent had an ACE score of 0, compared with 9 percent of those who grew up with two alcohol-abusing parents. Six percent of the former group had an ACE score of 4 or more, compared with 39 percent of the latter group. After adjustment for age, race, sex, and education, the mean±SD ACE scores according to parental history of alcohol abuse were as follows: neither parent, 1.2±.04; mother only, 2.5±.10; father only, 2.1±.05; and both parents, 2.9±.09. Differences between all groups were statistically significant in the linear regression analysis (p<.001).
As can be seen in Table 3, a personal history of alcoholism was reported by 5.8 percent of respondents (N=539), a lifetime history of depression was reported by 23.1 percent (N=2,159), and recent problems with depressed affect by 23.4 percent (N=2,184). Each of the nine adverse childhood experiences was associated with both personal alcoholism (p<.05), a lifetime history of depression (p<.05), and recent problems with depressed affect (p<.05).
As shown in the individual models in Table 4, a personal history of alcoholism was strongly related to having alcohol-abusing parents and to the number of adverse childhood experiences reported. We concluded that these two factors were independent, because each remained strongly associated with having a personal history of alcoholism after we simultaneously adjusted for both in the statistical model (fully adjusted model in Table 4). Indeed, the overall fit of the logistic regression model in which only parental alcohol abuse was considered was significantly improved when the ACE score was added (χ2=67, df=4, p<.001). This result suggests that the most accurate estimate of the relationship between having a personal history of alcoholism and either of these factors is obtained when both are accounted for simultaneously.
The individual model in Table 4 suggests that parental alcohol abuse increased the risk of depression by 30 to 50 percent. However, having alcohol-abusing parents was not independently associated with a lifetime history of depression after we adjusted for the ACE score. The odds ratios for having alcohol-abusing parents were all near the null value of 1, whereas the odds ratios for the ACE score were strong and graded. Further evidence that adverse childhood experiences are important risk factors for depression comes from the finding that the fit of the model that included only parental alcohol abuse was dramatically improved with the addition of the ACE score (χ2=2=447, df=4, p<.001). The addition of both the ACE score and a personal history of alcoholism did not improve the fit of the model (data not shown). The findings for depressed affect in the past year were nearly identical to those for a lifetime history of depression (data not shown).
Respondents with higher ACE scores were more likely to have a personal history of alcoholism. Furthermore, among respondents with similar ACE scores, the prevalence of alcoholism was substantially higher among those who had alcohol-abusing parents than among those who did not. We fit a generalized linear model with binomial errors and identity link to the prevalence data and found no evidence that parental alcohol abuse modified the relationship between ACE score and a personal history of alcoholism.
Although we found a strong, graded relationship between the ACE score and a lifetime history of depression, we did not find that depression was more prevalent among respondents who had alcohol-abusing parents. We fit a generalized linear model with binomial errors and identity link to the prevalence data and found no evidence that parental alcohol abuse modified the relationship between ACE score and current depression. The findings for the variable "depressed affect in the past year" were nearly identical to those for current depression.
Discussion
Growing up with alcohol-abusing parents substantially increased the risk of each of the nine adverse childhood experiences as well as the risk of multiple adverse experiences. We found an independent, graded relationship between the number of adverse childhood experiences reported and the risk of alcoholism and depression regardless of whether the respondent reported parental alcoholism. Although the prevalence of personal alcoholism was higher among respondents with a parental history of alcoholism, parental history did not affect the strength of the graded relationship between the ACE score and alcoholism. An important finding of this study is that depressive disorders among adult children of alcoholics appear to be largely, if not solely, due to the greater likelihood of having had adverse childhood experiences in a home with alcohol-abusing parents. Respondents who had similar ACE scores had a similar risk of depression—both lifetime and current—whether or not they had alcohol-abusing parents.
Other studies have shown that childhood trauma and familial and genetic factors are associated with alcoholism and other forms of substance abuse (29,45,46,47). Family studies have found that adult children of alcoholics are three or four times as likely to develop alcoholism as adults whose parents were not alcoholics (29). Twin studies have found concordance rates of alcoholism of between 30 percent and 36 percent among fraternal twins and 60 percent among identical twins (48). Similarly, adopted sons of alcoholic fathers have a higher risk of alcoholism than adopted sons of nonalcoholic fathers (49).
The increased risk of alcoholism reported in these studies is consistent with our finding of a 3.5- to 5.6-fold risk of alcoholism among adult children of alcoholics regardless of the extent to which they had adverse childhood experiences. Previously published findings from the Adverse Childhood Experiences Study have also shown that adults who reported four or more adverse childhood experiences were two to ten times as likely as adults who had no adverse childhood experiences to report other forms of substance abuse, including illegal drug use, parenteral drug abuse, and smoking (9,10). Another area of research that is still in its infancy has identified physiologic and biochemical markers of familial transmission of alcoholism (29,50,51).
The aggregation of alcoholism and depressive disorders in families has been observed (52,53), but its underlying mechanism is unclear. We found that depressive disorders were 30 percent to 50 percent more common among adult children of alcoholics, a finding consistent with a previous report (54). However, we also observed that parental alcoholism was not independently related to lifetime risk of current depression after we simultaneously controlled for adverse childhood experiences and a personal history of alcoholism. Furthermore, we found no evidence that adverse childhood experiences and parental alcoholism interact to increase the risk of depression. Rather, the increased risk of depression among adult children of alcoholics appears to have been determined by the extent of childhood trauma, such as abuse, domestic violence, and other family dysfunction, that we found to be substantially more common in alcoholic households.
Our results corroborate previous findings suggesting that traumatic childhood experiences are an important component in the etiology of alcoholism and depression (29,47,55,56,57,58,59,60,61,62,63,64,65,66,67). Understanding that the origins of depression among adult children of alcoholics may be the result of the trauma of child abuse, domestic violence, and other family dysfunction could be critical to the diagnosis and treatment of depression in this group (9,47,67).
Adverse childhood experiences such as sexual abuse have been shown to be underreported (68,69). Furthermore, our measure of personal alcoholism likely resulted in substantial underreporting of a personal history of alcoholism. These forms of underreporting probably would have biased our results toward the null hypothesis, and thus our estimates of the association between adverse childhood experiences and both depression and alcoholism are probably conservative.
Our study showed that the risk of mental illness, drug abuse, and suicide attempts in the household was strongest when the mother was an alcoholic and that the risk did not significantly increase when both parents were alcoholics. The pivotal role of an alcoholic mother in the emergence of household dysfunction may stem from the fact that the mother is generally the primary caretaker. Alcohol abuse may diminish a mother's capacity to care for her children and to deal with household problems. In addition, women who abuse alcohol are more likely to marry chemically dependent men (70). An alcoholic mother's difficulty in caring for her children may be exacerbated by the coexistence of affective, personality, and thought disorders (53).
Our findings suggest that prevention of child abuse, domestic violence, and other forms of household dysfunction that are common in alcoholic families will depend on advances in the identification and treatment of alcoholic parents (4,6,7,54). Improved recognition and treatment of alcoholism in adults and tandem family interventions to reduce the burden of adverse childhood experiences in alcoholic households (9,10) would probably decrease the long-term risk of alcoholism, depression, and other adverse effects of trauma observed among adult children of alcoholics (54,71,72,73,74). Alcohol treatment programs and child protective and welfare services have tended to ignore the likelihood that they share a population of clients (1,47). The tendency is probably even more pronounced in primary care settings, where despite guidelines established by the American Medical Association (75,76,77), clinicians' inquiries about issues such as domestic violence are infrequent (47,78,79,80).
Health care providers need training and guidelines not only for identifying and treating families in which children are exposed to adverse experiences but also for identifying and treating adult children of alcoholics (81,82,83). Our data strongly suggest that prevention and treatment of alcohol abuse and depression, especially among adult children of alcoholics, will depend on clinicians' inquiring about parental alcohol abuse and the long-term effects of adverse childhood experiences, with which both alcohol abuse and depression are strongly associated.
Acknowledgments
The authors thank Naomi Howard, B.A., for her efforts to make the adverse childhood experiences study possible. The study was supported under cooperative agreement TS-44-10/11 from the Centers for Disease Control and Prevention through the Association of Teachers of Preventive Medicine and a grant from the Garfield Memorial Fund. Ms. Dube was supported by cooperative agreement TS-44-10/11 from the Centers for Disease Control and Prevention through the Association of Teachers of Preventive Medicine.
Dr. Anda, Dr. Chapman, Dr. Edwards, Ms. Dube, and Dr. Williamson are affiliated with the National Center for Chronic Disease Prevention and Health Promotion of the Centers for Disease Control and Prevention in Atlanta. Dr. Whitfield is in private practice in Atlanta, and Dr. Felitti is with the department of preventive medicine at Southern California Permanente Medical Group (Kaiser-Permanente) in San Diego. Send correspondence to Ms. Dube, Mailstop K-47, Centers for Disease Control and Prevention, 4770 Buford Highway, N.E., Atlanta, Georgia 30341-3724 (e-mail, [email protected]).
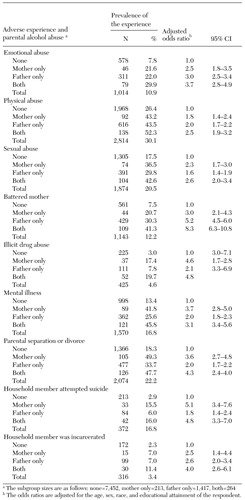 |
Table 1. Prevalence and risk of nine adverse childhood experiences among 9,346 adults with and without a history of parental alcohol abuse
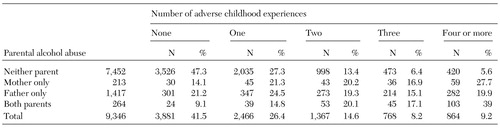 |
Table 2. Relationship between parental alcohol abuse and the number of adverse childhood experiences
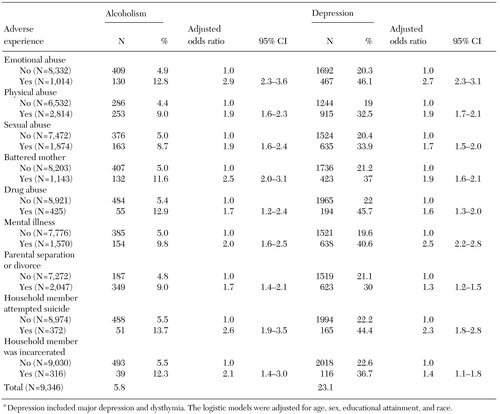 |
Table 3. Relationship between adverse childhood experiences and the prevalence and risk of lifetime or current alcoholism or depressiona
a Depression included major depression and dysthymia. The logistic models were adjusted for age, sex, educational attainment, and race.
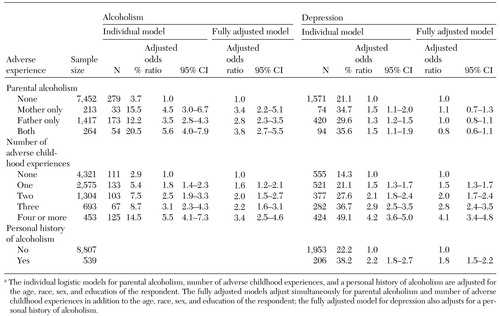 |
Table 4. Relationship of parental alcohol abuse to the prevalence and risk of current or lifetime alcoholism and depression with and without control for adverse childhood experiencesa
a The individual logistic models for parental alcoholism, number of adverse childhood experiences, and a personal history of alcoholism are adjusted for the age, race, sex, and education of the respondent. The fully adjusted models adjust simultaneously for parental alcoholism and number of adverse childhood experiences in addition to the age, race, sex, and education of the respondent; the fully adjusted model for depression also adjusts for a personal history of alcoholism.
1. Woodside M: Policy issues and action: an agenda for children of substance abusers, in Children of Chemically Dependent Parents: Perspectives From the Cutting Edge. Edited by Rivinus TM. New York: Brunner/Mazel, 1991Google Scholar
2. Grant BF: Estimates of US children exposed to alcohol abuse and dependence in the family. American Journal of Public Health 90:112-115, 2000Crossref, Medline, Google Scholar
3. Whitfield CL: Memory and Abuse: Remembering and Healing the Effects of Trauma. Deerfield Beach, Fla, Health Communications, 1995Google Scholar
4. Whitfield CL: Treatment issues for children of alcoholics. NIAAA First National Symposium on Services to Children of Alcoholics. NIAAA Research Monograph 4. DHHS pub ADM81-1007. Rockville, Md, National Institute of Alcohol Abuse and Alcoholism, 1981Google Scholar
5. Rudy DR: The Adult Children of Alcoholics movement: a social constructionist perspective, in Society, Culture, and Drinking Patterns Reexamined. Edited by Pittman DJ, White HR. New Brunswick, NJ, Rutgers Center of Alcohol Studies, 1991Google Scholar
6. Humphreys K: World view change in Adult Children of Alcoholics/Al-Anon self-help groups: reconstructing the alcoholic family. International Journal of Group Psychotherapy 46:255-263, 1996Crossref, Medline, Google Scholar
7. Black C: It Will Never Happen to Me! New York, Ballantine, 1981Google Scholar
8. Jacob T, Seilhamer RA: Alcoholism and family interaction, in Family Interaction and Psychopathology: Theories, Methods, and Findings. Edited by Jacob T. New York, Plenum, 1987Google Scholar
9. Felitti VJ, Anda RF, Nordenberg D, et al: The relationship of adult health status to childhood abuse and household dysfunction. American Journal of Preventive Medicine 14:245-258, 1998Crossref, Medline, Google Scholar
10. Anda RF, Croft JB, Felitti VJ, et al: Adverse childhood experiences and smoking during adolescence and adulthood. JAMA 282:1652-1658, 1999Crossref, Medline, Google Scholar
11. Fox KM, Gilbert B: The interpersonal and psychological functioning of women who experienced childhood physical abuse, incest, and parental alcoholism. Child Abuse and Neglect 18:849-858, 1994Crossref, Medline, Google Scholar
12. Fleming J, Mullen P, Bammer G: A study of potential risk factors for sexual abuse in childhood. Child Abuse and Neglect 21:49-58, 1997Crossref, Medline, Google Scholar
13. Wolock I, Magura S: Parental substance abuse as a predictor of child maltreatment. Child Abuse and Neglect 20:1183-1193, 1996Crossref, Medline, Google Scholar
14. Dore MM, Doris JM, Wright P: Identifying substance abuse in maltreating families: a child welfare challenge. Child Abuse and Neglect 19:531-543, 1995Crossref, Medline, Google Scholar
15. Ethier LS, Lacharite C, Couture G: Childhood adversity, parental stress, and depression of negligent mothers. Child Abuse and Neglect 19:619-632, 1995Crossref, Medline, Google Scholar
16. Spaccarelli S, Coatsworth JD, Bowden BS: Exposure to family violence among incarcerated boys: its association with violent offending and potential mediating variables. Violence and Victimization 10:163-182, 1995Crossref, Medline, Google Scholar
17. McCloskey LA, Figueredo AJ, Koss MP: The effects of systemic family violence on children's mental health. Child Development 66:1239-1261, 1995Crossref, Medline, Google Scholar
18. Brent DA, Perper JA, Moritz G, et al: Familial risk factors for adolescent suicide: a case-control study. Acta Psychiatrica Scandinavica 89:52-58, 1994Crossref, Medline, Google Scholar
19. Shaw DS, Vondra JI, Hommerding KD, et al: Chronic family adversity and early child behavior problems: a longitudinal study of low income families. Journal of Child Psychology and Psychiatry 35:1109-1122, 1994Crossref, Medline, Google Scholar
20. Zeitlen H: Children with alcohol misusing parents. British Medical Journal 50:139-151, 1994Google Scholar
21. West MO, Prinz RJ: Parental alcoholism and childhood psychopathology. Psychological Bulletin 102:204-218, 1987Crossref, Medline, Google Scholar
22. Merikangas KR, Dierker LC, Szatmari P: Psychopathology among offspring of parents with substance abuse and/or anxiety disorders: a high-risk study. Journal of Child Psychology and Psychiatry and Allied Disciplines 39:711-720, 1998Crossref, Medline, Google Scholar
23. Nordberg L, Rydelius PA, Zetterstrom R: Children of alcoholic parents: health, growth, mental development, and psychopathology until school age: results from a prospective longitudinal study of children from the general population. Acta Paediatrica 387(suppl)1-24, 1993Google Scholar
24. Steinhausen HC, Gobel D, Nester V: Psychopathology in the offspring of alcoholic parents. Journal of the American Academy of Child and Adolescent Psychiatry 23:465-471, 1984Crossref, Google Scholar
25. Henderson MC, Albright JS, Kalichman SC, et al: Personality characteristics of young adult offspring of substance abusers: a study highlighting methodologic issues. Journal of Personality Assessment 63:117-134, 1994Crossref, Medline, Google Scholar
26. Steinhausen HC: Children of alcoholic parents: a review. European Child and Adolescent Psychiatry 4:143-152, 1995Crossref, Medline, Google Scholar
27. Cloninger CR, Bohman M, Sigvardsson S: Inheritance of alcohol abuse. Archives of General Psychiatry 38:861-868, 1981Crossref, Medline, Google Scholar
28. Kapiro J, Koshenvuo M, Langinvainio H, et al: Genetic influences on use and abuse of alcohol: a study of 5,638 adult Finnish twin brothers. Alcoholism 11:349-356, 1987Crossref, Google Scholar
29. Cotton NS: The familial incidence of alcoholism: a review. Journal of Studies on Alcohol 40:89-116, 1979Crossref, Medline, Google Scholar
30. Anthenelli RM, Schuckit MA: Genetics, in Substance Abuse: A Comprehensive Textbook, 3rd ed. Edited by Lowinson JH. Baltimore, Williams & Wilkins, 1997Google Scholar
31. Schuckit MA: New findings in the genetics of alcoholism. JAMA 281:1875-1876, 1999Crossref, Medline, Google Scholar
32. Edwards VJ, Anda RF, Nordenberg DF, et al: Bias assessment for child abuse survey; factors affecting probability of response to a survey about childhood abuse. Child Abuse and Neglect 25:307-312, 2001Crossref, Medline, Google Scholar
33. Schoenborn CA: Exposure to Alcoholism in the Family: United States, 1988. Advance Data no 205. Vital Health Statistics 16(21). DHHS pub PHS95-1880.Hyattsville, Md, National Center for Health Statistics, 1995Google Scholar
34. Straus M, Gelles RJ: Physical Violence in American Families: Risk Factors and Adaptations to Violence in 8,145 Families. New Brunswick, NJ, Transaction Press, 1990Google Scholar
35. Wyatt GE: The sexual abuse of Afro-American and white American women in childhood. Child Abuse and Neglect 9:507-519, 1985Crossref, Medline, Google Scholar
36. Dietz PM, Spitz AM, Anda RF, et al: Unintended pregnancy among adult women exposed to abuse or household dysfunction during their childhood. JAMA 282:1359-1364, 1999Crossref, Medline, Google Scholar
37. Hillis SD, Anda RF, Felitti VJ, et al: Adverse childhood experiences and sexually transmitted diseases in men and women: a retrospective study. Pediatrics 106(1):E11, 2000Google Scholar
38. Wells KB: Depression as a Tracer Condition for the National Study of Medical Care Outcomes. Santa Monica, Calif, Rand, 1985Google Scholar
39. Burnam MA, Wells KB, Leake B, et al: Development of a brief screening instrument for detecting depressive disorders. Medical Care 26:775-789, 1988Crossref, Medline, Google Scholar
40. Burnam MA, Hough RL, Escobar JL, et al: Six-month prevalence of specific psychiatric disorders among Mexican-Americans and non-Hispanic whites in Los Angeles. Archives of General Psychiatry 44:687-694, 1987Crossref, Medline, Google Scholar
41. Hough RL, Landsverk JA, Stone JD, et al: Psychiatric Screening Scale Project: Final Report. Contract DB-81-0036. Rockville, Md, National Institutes of Mental Health, 1983Google Scholar
42. Robins LN, Helzer JE, Groughan J, et al: National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Archives of General Psychiatry 38:381-389, 1981Crossref, Medline, Google Scholar
43. Roberts RE, Vernon SW: The Center for Epidemiologic Studies Depression Scale: its use in a community sample. American Journal of Psychiatry 140:41-46, 1983Link, Google Scholar
44. Rothman KJ: Modern Epidemiology. Boston, Little, Brown, 1986Google Scholar
45. McGue M: A behavioral-genetic perspective on children of alcoholics. Alcohol Health and Research World. 21:210-217, 1997Google Scholar
46. Whitfield CL: Internal evidence and corroboration of traumatic memories of child sexual abuse with addictive disorders. Sexual Addiction an Compulsivity 5:269-292, 1998Crossref, Google Scholar
47. Substance Abuse Treatment for Persons With Child Abuse and Neglect Issues. Treatment Improvement Protocol 36. Rockville, Md, Center for Substance Abuse Treatment, 2000Google Scholar
48. Cadoret RJ, Yates WR, Troughton E, et al: An adoption study of genetic and environmental factors in drug abuse. Archives of General Psychiatry 43:1131-1136, 1986Crossref, Medline, Google Scholar
49. Cermak TL: Evaluating and Treating Adult Children of Alcoholics: Vol 1. Evaluation. Minneapolis, Johnson Institute, 1990Google Scholar
50. Nixon SJ, Tivis LJ : Neuropsychological responses in children of alcoholics. Alcohol Health and Research World 21:232-236, 1997Medline, Google Scholar
51. Porjesz B, Begleiter H: Event-related potentials in CoAs. Alcohol Health and Research World 21:236-240, 1997Medline, Google Scholar
52. Ellis DA, Zucker RK, Fitzgerald HE: The role of family influences in development and risk. Alcohol Health and Research World 21:218-226, 1997Medline, Google Scholar
53. Klerman GL, Weissman MM, Rounsaville BJ, et al: Interpersonal Psychotherapy of Depression: A Brief, Focused, Specific Strategy. Northvale, NJ, Aronson, 1984Google Scholar
54. An Assessment of the Needs of and Resources for Children of Alcoholic Parents: An Extensive Interview Study of 50 CoAs. Rockville, Md, National Institute of Alcohol Abuse and Alcoholism, 1974Google Scholar
55. Root M: Treatment failures: the role of sexual victimization in women's addictive behavior. American Journal of Orthopsychiatry 59:542-549, 1989Crossref, Medline, Google Scholar
56. Wallen J, Berman K: Possible indicators of childhood sexual abuse for individuals in substance abuse treatment. Journal of Child Sexual Abuse 1:63-74, 1992Crossref, Google Scholar
57. Ladwig GB, Anderson MD: Substance abuse in women: relationship between chemical dependency in women and past reports of physical and sexual abuse. International Journal of the Addictions 24:739-744, 1989Crossref, Medline, Google Scholar
58. Kaufman J: Depressive disorders in maltreated children. Journal of the American Academy of Child and Adolescent Psychiatry 30:257-265, 1991Crossref, Medline, Google Scholar
59. Herman JL: Trauma and Recovery. New York, Basic Books, 1992Google Scholar
60. Lowenstein RJ: Somatoform disorders in victims of incest and child abuse, in Incest-Related Syndromes of Adult Psychopathology. Edited by Kluft R. Washington, DC, American Psychiatric Press, 1990Google Scholar
61. Walker E, Katon W, Harrop-Griffiths J, et al: Relationship of chronic pelvic pain to psychiatric diagnoses and childhood sexual abuse. American Journal of Psychiatry. 145: 75-80, 1988Google Scholar
62. Morrison J: Childhood sexual histories of women with somatization disorder. American Journal of Psychiatry 146:239-241, 1989Link, Google Scholar
63. Bryer JB, Nelson BA, Miller JB, et al: Childhood sexual and physical abuse as factors in adult psychiatric illness. American Journal of Psychiatry 144:1426-1430, 1987Link, Google Scholar
64. Felitti VJ: Childhood sexual abuse, depression, and family dysfunction in adult obese patients. Southern Medical Journal 86:732-736, 1993Crossref, Medline, Google Scholar
65. Felitti VJ: Long-term medical consequences of incest, rape, and molestation. Southern Medical Journal 83:328-331, 1991Crossref, Google Scholar
66. Evans K, Sullivan J: Treating Addicted Survivors of Trauma. New York, Guilford, 1995Google Scholar
67. Briere J: Therapy for Adults Molested as Children: Beyond Survival, 2nd ed. New York, Springer, 1996Google Scholar
68. Femina DD, Yeager CA, Lewis DO: Child abuse: adolescent records vs adult recall. Child Abuse and Neglect 14:227-231, 1990Crossref, Medline, Google Scholar
69. Williams LM: Recovered memories of abuse in women with documented child sexual victimization histories. Journal of Traumatic Stress 8:649-673, 1995Crossref, Medline, Google Scholar
70. Ellis DA, Zucker RA, Fitzgerald HE: The role of family influences in development and risk. Alcohol Health and Research World 21:218-226, 1997Medline, Google Scholar
71. Whitfield CL: Healing the Child Within: Discovery and Recovery for Adult Children of Dysfunctional Families. Deerfield Beach, Fla, Health Communications, 1987Google Scholar
72. Gravitz H, Bowden J: Guide to Recovery for ACoAs. Holmes Beach, Fla, Learning Publications, 1985Google Scholar
73. Brown S: Treating Adult Children of Alcoholics: A Developmental Perspective. NY, Wiley, 1988Google Scholar
74. Rivinus TM: Children of Chemically Dependent Parents. NY, Brunner/Mazel, 1991Google Scholar
75. Council on Scientific Affairs: American Medical Association Diagnostic and Treatment Guidelines on Domestic Violence. Archives of Family Medicine 1:38-47, 1992Google Scholar
76. Council on Scientific Affairs: AMA diagnostic and treatment guidelines concerning child abuse and neglect. JAMA 254:796-800, 1985Crossref, Medline, Google Scholar
77. Sugg NK, Inui T: Primary care physicians' response to domestic violence: opening Pandora's box. JAMA 267:3157-3160, 1992Crossref, Medline, Google Scholar
78. Hamberger LK, Saunders DG, Hovey M: Prevalence of domestic violence in community practice and rate of physician inquiry. Family Medicine 24:283-287, 1992Medline, Google Scholar
79. Friedman LS, Samet JH, Roberts MS, et al: Inquiry about victimization experiences: a survey of patient preferences and physician practices. Archives of Internal Medicine 152:1186-1190, 1992Crossref, Medline, Google Scholar
80. Krugman RD: Future role of the pediatrician in child abuse and neglect. Pediatric Clinics of North America 37:1003-1011, 1990Crossref, Medline, Google Scholar
81. Dubowitz H: Child abuse programs and pediatric residency training. Pediatrics 82:477-480, 1988Medline, Google Scholar
82. Alpert EJ, Tonkin AE, Seeherman AM, et al: Family violence curricula in US medical schools. American Journal of Preventive Medicine 14:273-282, 1998Crossref, Medline, Google Scholar
83. Short LM, Johnson D, Osattin A: Recommended components of health care provider training programs on intimate partner violence. American Journal of Preventive Medicine 142:283-288, 1998Crossref, Google Scholar



